Introducing Industrialized CRISPR Cells, Powered by the Eclipse™ Platform

Contents
In this episode of CRISPR Cuts, we converse with Dr. Jesse Boehm, principal investigator at the Broad Institute and Chief Science Officer of Break Through Cancer. Dr. Boehm has spent the last fifteen years at the Broad Institute’s Cancer program as an institute scientist and a lead scientist on the Cancer Dependency Map project. The Cancer Dependency Map project is a good example of the power of collaborative team science.
Now, Dr. Boehm and his colleagues have formed a new Foundation called Break Through Cancer—a collaboration between MIT's Koch Institute, Dana Farber Cancer Institute, MD Anderson, Memorial Sloan Kettering, and Johns Hopkins Medicine. Scientists from these institutes have come together for a multi-institutional and patient-centric research project to combat mankind’s most feared disease amidst a worldwide pandemic.
Check out the CRISPR Cuts episode featuring Dr. Boehm, and read the summary below.
Need for Precision Medicine in Cancer Treatment & Cancer Dependency Map
Minu: What type of projects do you currently work on at the Broad Institute?
Dr. Boehm: We're trying to figure out how to kill cancer cells, which seems like a very routine, simple-minded sort of question, but it's really the essence of making precision cancer medicine a reality. We all imagine a future in which a patient could go to their doctor, the doctor could read off of the molecular profile of the tumor and would tell the patient, "Here are the drugs or the combination of drugs that are predicted to be useful in your tumor with your genetic fingerprint."
This concept of precision medicine treatment is working for around 25% of cancer patients today, but it's not working for everyone because in most cases, even when we get the genetics of a patient's tumor, we can't decide exactly what drugs to give them.
My work at the Broad Institute over the last 15 years is to try to use laboratory technologies to solve that challenge. This includes growing cells from patient's tumors and then using every drug that's ever been created for any disease and using CRISPR technology to cut every gene one by one, even if we don't have a drug. We are trying to figure out in the lab what are the vulnerabilities of every type of cancer growing in dishes. We call this project a Cancer Dependency Map.
"This is kind of like Google maps; it might tell you what are the weak points in the traffic patterns to help you get to work. The dependency map is aimed at finding all of the Achilles heels of every type of cancer in the lab. We think that will be a foundational starting point for drug companies everywhere to choose the best targets to go after for the next generation of cancer therapies."
- Dr. Jesse Boehm, PI at the Broad Institute
What is the Break Through Cancer Effort
Minu: What is the Break Through Cancer Foundation and what are you currently focusing on?
Dr. Boehm: Over the last 15 years at the Broad, we've seen the amazing potential for team-based science. How do you get scientists from different labs, from different organizations, maybe even from different countries to work together seamlessly, to identify a really big challenge blocking the field, and incentivize them to work together to address that challenge?
There's never been so much collaboration for cancer, and we're just very excited that the Broad Institute has played a small role in that.
Several years ago, a family identified a new opportunity and agreed to donate $250 million to try to stimulate a similar flavor of team-based cancer research, not only in the Boston area but across the nation. This family aspired for teams to come together to try to build out team-based cancer projects across these five organizations in much the same way that the Broad Institute and many others had shown was possible locally. Starting with five leading cancer centers, Dana-Farber in Boston, MIT in Cambridge, Mass, MD Anderson in Texas, Memorial Sloan Kettering in New York City, and Johns Hopkins in Baltimore, we built the Break Through Cancer Foundation.
A really long time ago, prior to the COVID pandemic, we sort of thought it was really difficult to make team-based science projects because everyone wanted to collaborate based on physical proximity and people that they trust and are comfortable with, but we've all woken up from the fog. The pandemic has left us totally in awe of what's been possible across nations, across countries, using virtual tools for scientists to come together and just tackle amazingly impossible challenges, making COVID vaccines and under a year, solving intricacies of the COVID virus. Over the next few months, we plan to fund serious projects, $20 million or more in a number of cancer types to try to solve really attractive or even impossible-sounding challenges.
So I'm really excited about the organization launching at this just unprecedented moment for international science. It couldn't have been a better time.
We're trying to capitalize on that opportunity with this new foundation called Break Through Cancer, to utilize the same sense of urgency that the international scientific community felt for COVID and to bring that urgency to team-based collaboration in cancer.
Minu: Is Break Through Cancer Foundation focused on the discovery part of cancer or will it also focus on patient treatments or trials?
Dr. Boehm: The overarching scope is to try to bring the worlds of clinical cancer science and laboratory cancer science closer together than ever before and to put patients at the center. We think scientists work on cells, mice, and other organisms, but more than anything we should be learning from every patient's experience. We aim to utilize patient samples and bring those to the lab, and use technologies like CRISPR to figure out what happened in the clinic and why did it happen mechanistically?
We're realizing that there are types of their journeys, their archetypes of scientific inquiry that most scientists would like just to be routine and actually most patients and families probably assume are routine, including a scientist comes up with a hypothesis in the lab and very quickly test that in a patient to see if it's right and then utilizes some next-generation technology to figure out, did they get the answer correct? That concept of moving quickly between the lab and the clinic is just not actually happening. It is usually only 5% of ideas from the lab that are even tested in patients. To get one idea tested might take 10 years to organize. You have to know the right people and raise the right money. This is goal number one.
Goal number two is to intervene as early as possible. Cancers are often detected late and it's often too late to intervene. There are already billions of cells and even if you kill tens of millions of them, there are still tens of millions left behind. So can we shift the curve and find individuals that are at high risk using genetics or other tools that are just walking around and monitor them much more closely and then intervene whether that's through the vaccination, or therapeutics, or something else so that they never develop late-stage cancer.
So we're challenging teams to come up with projects that align with those two conceptual areas of framework and we call those Break Through Cancer project archetypes.
Impact of CRISPR technology on Cancer Therapy & Research
Minu: Let's talk about how the introduction of CRISPR is shaping this field or changing the course of the field. How is CRISPR impacting cancer research?
Dr. Boehm: CRISPR has fundamentally changed everything essentially overnight. I think CRISPR is often viewed as a potential therapeutic tool. We're seeing CRISPR having a transformative effect in the laboratory as a cancer research tool.
The reproducibility of discoveries using CRISPR is high and results across labs are much more overlapping than ever before. We undertook a major set of analyses with our colleagues at the Sanger Institute in the United Kingdom, who did a similar type of cancer dependency work. We found that the two data sets using CRISPR were highly reproducible. With so much more data and much more reproducibility, CRISPR has democratized access to this type of genome engineering technology.
Cancer Cell Lines and How CRISPR is Transforming Cancer Research
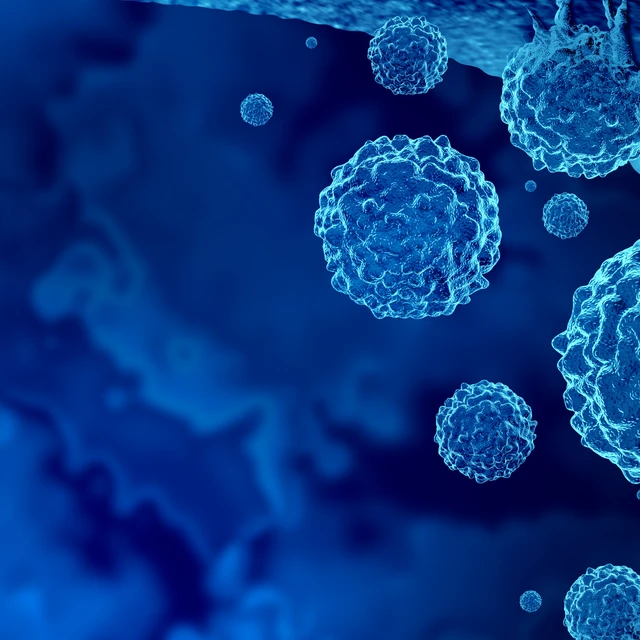
Ten years ago, it would've been very difficult to find all the ways that a drug becomes resistant to therapy or find all of the vulnerabilities in the cancer cell. Now, any lab can do this. The uptake of CRISPR technology was the fastest uptake of any new technology. I think what's often overlooked in the media is just the incredible change that's happening to preclinical research and those activities will lead to better, more accurate, more efficacious, and more successful drugs in the near future.
Instead of cancer drug discovery companies working on random targets that they think are interesting, they can just look up in the dependency map what are the best targets. I think we're going to find in a couple of decades that cancer drug development will be more successful, perhaps cheaper and with better patient selection because of all of the advances of CRISPR in the laboratory. It's completely exciting and thrilling to be part of this at this moment.
CRISPR-Edited Engineered Cells
Stop using CRISPR. Start Doing CRISPR. Synthego’s Engineered Cells allow you to focus on discoveries.
How Large-Scale Disease Models Are Aiding Cancer Research
Minu: Recently we spoke with NIH scientists about their iNDI project, which is this large scale looking at hundreds of mutations in Alzheimer's. They basically created a set of disease models by just having all these variants done in different iPS cells. So how do you think about standardization of CRISPR or something like providing large-scale disease modeling cells, edited cells, how would that play out in cancer and how would that help Break Through Cancer Foundation or even your own work?
Dr. Boehm: The success of cancer research of course is predicated on having high-quality model systems. We are ultimately going to need around 10,000 or 20,000 cellular models in the lab to fully capture all of cancer. Today the field has about 2000. I see these two revolutions, one in growing tumors using organoid technology, and then using CRISPR to manipulate the genome in those organoids as being really key to ensuring we have a complete collection of cancer models by 2030.
This activity started at the Broad and has become an international network called the Human Cancer Models Initiative and there are labs across the US, the Netherlands, in Italy, in the United Kingdom, in Hinxton, UK, that are all working together to build out these new cellular models and importantly, to deposit these into a public database, ATCC, that allows researchers everywhere to access them. So we've created about 400 new cell models, we have sent around 300 of them to the distributor, and now researchers can begin accessing those models.
If your intention is to build resources like cellular models so that they can be shared infinitely with the entire globe, you need to start right at the beginning and engage patients in that process. We put online consent on the web, and we utilized a number of social media channels and Twitter and Facebook to advertise this. Patients started sending their samples and they started really being engaged in the project. Hundreds of samples from these rare tumor types came that wouldn't have come through ordinary mechanisms.
The Effect of COVID-19 on Collaborative Research
Minu: How did COVID impact your lab and collaborative projects?
Dr. Boehm: Prior to the COVID pandemic, we sort of thought it was really difficult to make team-based science projects work because everyone knows you only want to work with people that you know, who are in the lab next to you. We have all woken up from the fog of this kind of COVID pandemic in the last year and a half, just totally in awe of what's been possible across countries, using virtual tools for scientists to come together and tackle amazingly impossible challenges, making COVID vaccines and under a year, solving intricacies of the COVID virus.
We are trying to capitalize on that opportunity with this new foundation called Breakthrough Cancer, to utilize the same sense of urgency that the international scientific community felt for COVID and to bring that urgency to team-based collaboration in cancer. I am also excited about this organization launching at this just unprecedented moment for international science.
The utilization of collaborative research and revolutions in CRISPR technology, such as Break Through Cancer, has a realistic probability of success. For a disease as intricately complicated as cancer, there are no guarantees, but the effort to fight it needs to be just as intricately designed.