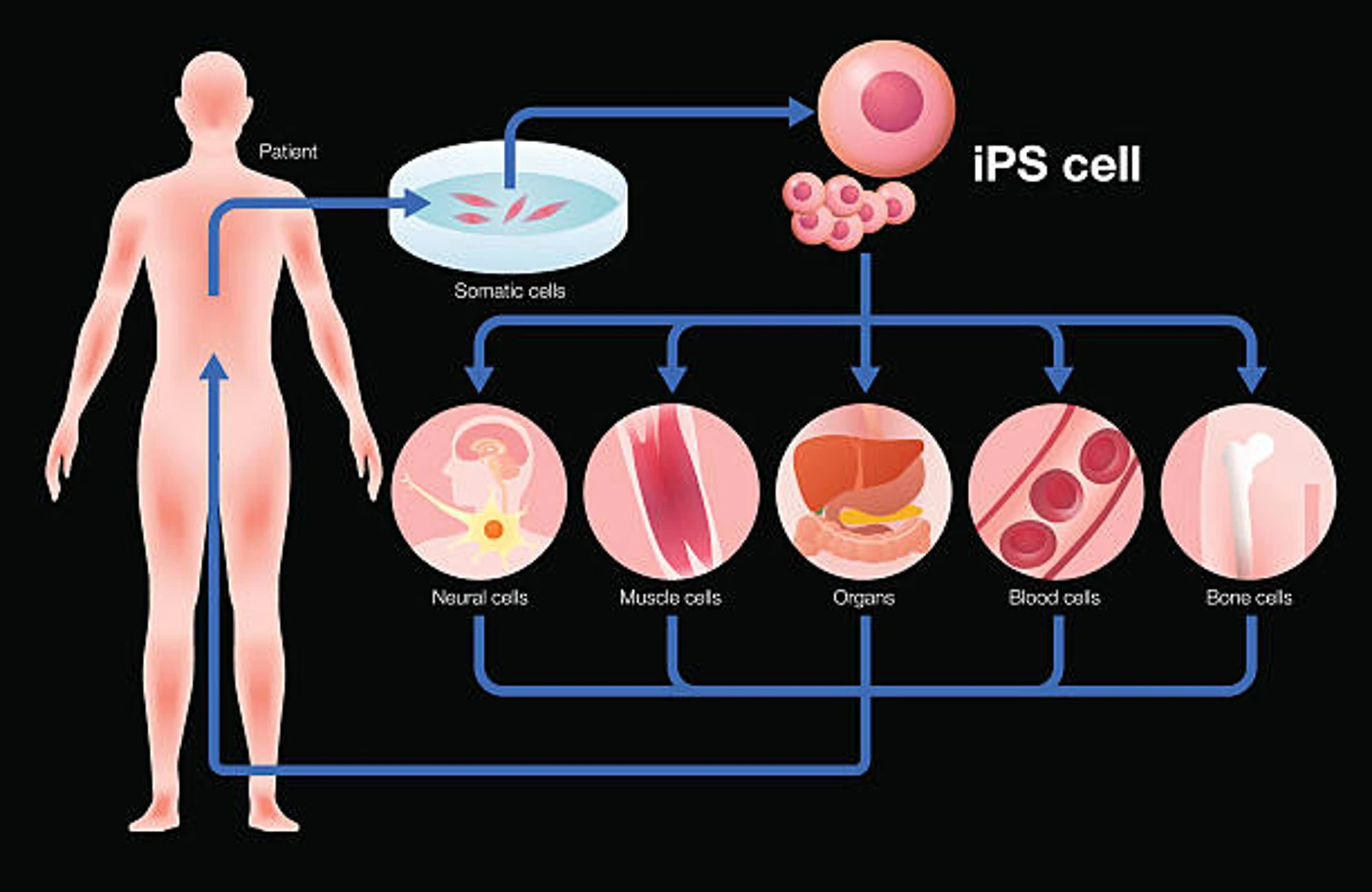
A clear application of iPSC CRISPR technology is functional genomics, the study of what genes do. At the time, researchers employed animal models or immortalized human cell lines to answer questions relating to gene function, using CRISPR or other gene editing technologies, to perform knockouts examining the effects of the edit on the phenotype, behavior, or physiology of the model. However, this approach is limited by the translatability of animal models, epigenetic factors, and the fact that many immortalized cell lines were originally isolated from tumors or harbor mutations.
CRISPR-edited iPS cells eliminate many of the confounding factors associated with these studies, allowing researchers to perform precision studies of gene function on any desired cell or tissue. This is because they can be used to generate isogenic cell lines that are genetically identical except for the particular disease-causing mutation of interest. This also makes these cells incredibly useful for generating much-needed precision models of human disease.
A major challenge in the field of cardiovascular disease research, for example, is to isolate and grow human primary cardiomyocytes used for disease modeling. CRISPR-edited iPSCs can be used to generate cardiomyocytes with specific disease-causing mutations, as well as to correct disease-causing mutations, with relative ease compared to previous methods. They were used in this context in a 2018 study of genomic variants of uncertain significance (VUS), employing the cells as an assessment tool to determine whether VUS are either pathogenic or benign.
They can also be used to generate other cell types involved in cardiovascular disease. For example, a 2017 study used CRISPR to knock out the lipase A (LIPA) gene in macrophages generated from iPSCs to determine the effect on cholesterol ester (CE) handling, efflux, and gene expression, all of which are involved in atherosclerotic cardiovascular disease.
CRISPR-edited iPSCs have also been used to generate much-needed models for studying neurological diseases, such as Alzheimer’s disease (AD), Parkinson’s Disease (PD), and Huntington’s Disease (HD), in which many genetic mutations are implicated. AD, for example, is frequently caused by E280A mutations in the Presenilin1 (PSEN1) gene. In 2019, researchers differentiated iPSCs into two identical neural cell lines, then used CRISPR to induce a homozygous PSEN1 mutation in one cell line and a heterozygous PSEN1 mutation in the other, creating two precision models for AD research.
A notable example use of iPSCs is the 2021 Inducible Pluripotent Stem Cell Neurodegeneration Initiative (iNDI). An initiative by the National Institute of Health (NIH), the iNDI project aimed to generate hundreds of disease models for Alzheimer’s Disease and Related Dementias (ADRD), making it the largest iPSC genome engineering study to date.
Another study generated multiple isogenic iPS cell lines and used them as models to study the effects of various genetic mutations in the leucine-rich repeat kinase 2 (LRRK2) gene, which are associated with inherited PD. The study utilized CRISPR-Cas9 to generate the fourteen cell lines, including both homozygous and heterozygous lines for five different LRRK2 pathogenic mutations, two lines carrying hypothesis-testing mutations, and two LRRK2 knockout lines. Studies like these provide valuable resources for neurological disease research.