CRISPR Revolution in Cell & Gene Therapy
Contents
Sickle cell disease affects nearly 100,000 Americans, and the global estimate is in the millions. The only viable treatment was a bone marrow transplant for several years, but advances in CRISPR gene therapy have recently created avenues for optimism. In this blog post, learn more about this disease and CRISPR cure directly from Jimi Olaghere, one of the early CRISPR clinical trial patients who has experienced complete recovery from his symptoms so far.
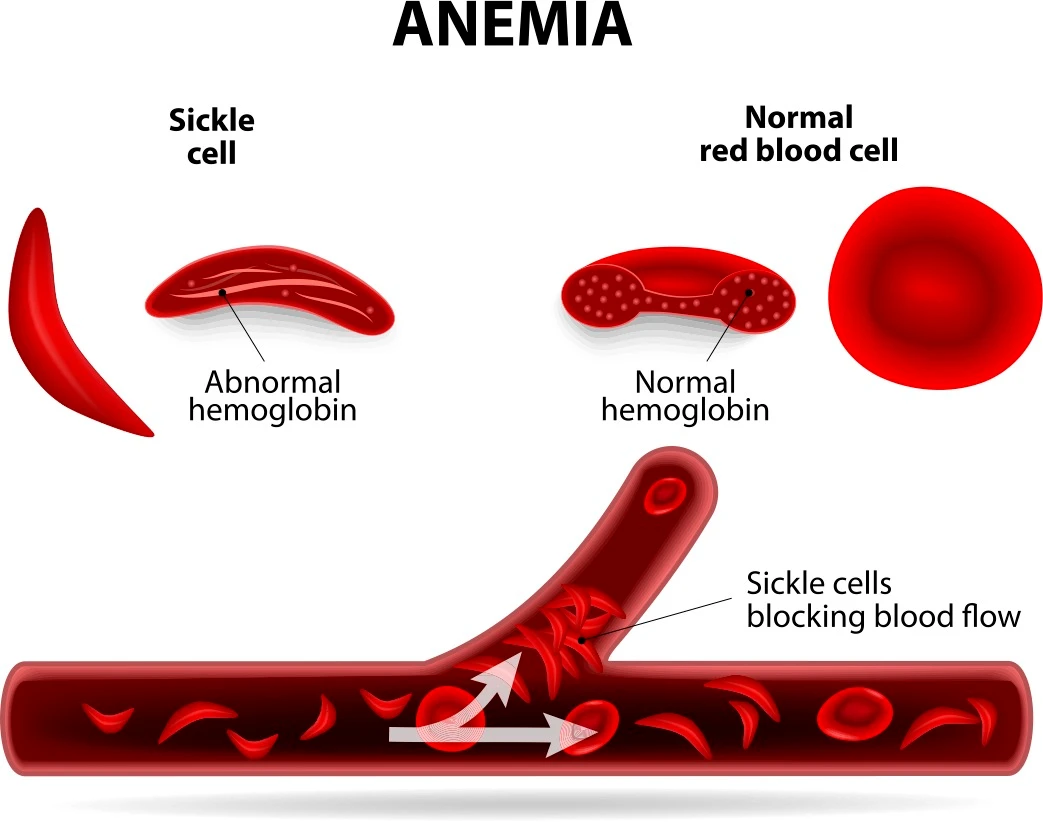
Sickle cell disease is a group of inherited blood disorders caused by a mutation in the gene encoding hemoglobin, the protein responsible for carrying oxygen in red blood cells. Red blood cells in normal healthy individuals are round in shape, flexible, and move easily through tiny blood vessels. Due to abnormal hemoglobin in this disease, these red blood cells become crescent-shaped or C-shaped in individuals affected with the condition and resemble a sickle. Hence the name sickle cell disease. Sickle cells are short-lived and do not move as easily through the blood vessels, often obstructing blood flow. This leads to chronic severe pain and other symptoms such as anemia, fatigue, and acute infections. To learn more about sickle cell disease and its management and the latest developments in the field, read this comprehensive guide.
Jimi Olaghere, an e-commerce entrepreneur, has lived with this disease all his life. In 2018, CRISPR Therapeutics and Vertex Pharmaceuticals joined forces to introduce a clinical trial for their CRISPR-based sickle cell therapy (CTX001). Jimi was one of the first few patients treated with this therapy.
In this interview on our CRISPR Cuts podcast, Jimi talks about his experiences as a sickle cell disease patient, his recent success with gene therapy trial and recovery, and how being cured of his symptoms has changed his life.
Listen to the entire podcast episode here:
5 Key Takeaways from Jimi’s Interview on Sickle Cell Disease and CRISPR CTX001 Therapy
1. Early Diagnosis and Challenges of Growing Up with Sickle Cell DiseaseSickle cell disease is inherited at birth, and the symptoms often start to show within the first year. Anemia and pain crisis or sickle crisis are the most common symptoms. Children with severe symptoms often find it challenging to have a normal childhood. Jimi opens up about his early memories of coming to terms with his diagnosis and experiences as a young sickle cell patient.
Time in podcast: 2:45
Sickle cell disease is inherited at birth, and the symptoms often start to show within the first year. Anemia and pain crisis or sickle crisis are the most common symptoms. Children with severe symptoms often find it challenging to have a normal childhood. Jimi opens up about his early memories of coming to terms with his diagnosis and experiences as a young sickle cell patient.
Time in podcast: 2:45
2. Navigating Life, Career, and Healthcare Systems as a Sickle Cell PatientIndividuals affected by sickle cell disease require constant care to manage their pain crises. This also means a substantial amount of their time is spent in hospitals and emergency rooms, waiting for medical attention. This impedes education, employment, and career opportunities and impacts their lives and families. Jimi shares his experiences as a young adult and how he navigated his path through the healthcare systems while trying to establish himself as a professional.
Time in podcast: 7:08
Individuals affected by sickle cell disease require constant care to manage their pain crises. This also means a substantial amount of their time is spent in hospitals and emergency rooms, waiting for medical attention. This impedes education, employment, and career opportunities and impacts their lives and families. Jimi shares his experiences as a young adult and how he navigated his path through the healthcare systems while trying to establish himself as a professional.
Time in podcast: 7:08
3. The Quest for Long-Term Treatment and Gene Therapy TrialWith new options for long-term therapies for sickle cell disease, patients can opt for multiple ways to manage and even cure their symptoms. Traditional long-term management approaches, including bone marrow transplants and stem cell transplants, requires complete or partial match with the donors and usually require very long recovery periods. Jimi explains how he learned about the gene therapy clinical trial and why he chose this as a treatment option.
Time in podcast: 12:54
With new options for long-term therapies for sickle cell disease, patients can opt for multiple ways to manage and even cure their symptoms. Traditional long-term management approaches, including bone marrow transplants and stem cell transplants, requires complete or partial match with the donors and usually require very long recovery periods. Jimi explains how he learned about the gene therapy clinical trial and why he chose this as a treatment option.
Time in podcast: 12:54
4. Undergoing CRISPR Gene-Editing Trial and RecoveryThe recent CRISPR gene therapy (CTX001) clinical trial for sickle cell disease (CLIMB SCD-121, funded by CRISPR Therapeutics and Vertex Pharmaceuticals) was found to be effective in the few early patients who had access to the treatment. Although in its early stages, the therapy seems to have no major adverse effects associated and has immensely improved the quality of life for affected individuals. Jimi talks about how this therapy has changed his life.
Time in podcast: 15:12
The recent CRISPR gene therapy (CTX001) clinical trial for sickle cell disease (CLIMB SCD-121, funded by CRISPR Therapeutics and Vertex Pharmaceuticals) was found to be effective in the few early patients who had access to the treatment. Although in its early stages, the therapy seems to have no major adverse effects associated and has immensely improved the quality of life for affected individuals. Jimi talks about how this therapy has changed his life.
Time in podcast: 15:12
5. Patient Advocacy, Creating Awareness and Hope for the CommunitySickle cell disease largely affects people of African descent. As an African American man who has experienced his entire life, until recently, through the lens of a sickle cell patient, Jimi feels obliged to give back to the community. He discusses how being cured of his symptoms has changed his outlook on life and how he is now motivated to share his story and mentor young children suffering from the disease.
Time in podcast: 28:59
Sickle cell disease largely affects people of African descent. As an African American man who has experienced his entire life, until recently, through the lens of a sickle cell patient, Jimi feels obliged to give back to the community. He discusses how being cured of his symptoms has changed his outlook on life and how he is now motivated to share his story and mentor young children suffering from the disease.
Time in podcast: 28:59
Diagnosis, Childhood, and Early SymptomsIn the following section, we will learn about Jimi’s experiences as a pediatric patient, coming to terms with his symptoms, and how that impacted his childhood and adolescent years.
In the following section, we will learn about Jimi’s experiences as a pediatric patient, coming to terms with his symptoms, and how that impacted his childhood and adolescent years.
Minu: Could you please tell us about yourself, your diagnosis, and how that impacted your early childhood?Jimi: I was diagnosed right at birth, but I didn't find out about my disease until I was a toddler. I remember not being in school and not being able to keep up with my friends in playing soccer, and often needing water breaks. I became sick of it, and one day I went home, and I asked my mom, and that's when she broke the news to me that I had this disease called sickle cell anemia.
I was disappointed because I knew that life seemed extra hard for me as a young toddler. It got me thinking about how life would be for me as a grown man if it were already impacting my life this much as a child. So, when I heard about the disease, I felt bleak.
Jimi: As I grew up, it became increasingly difficult to manage the crises. As a young man, I remember living in Nigeria and having no access to the emergency room and high-powered narcotics. I remember how painful those crises would feel; sometimes, I would pass out from pain and wake up the next morning. It just got worse growing up. Eventually, I moved to the US because I was born here, and we wanted to take advantage of the educational and healthcare system.
I remember my first crisis in the US, going to the emergency room and just being so in awe of how quickly a high-powered medication could alleviate my pain.
I remember coming here to the US excited and ambitious about what I would do and then just having to withdraw every semester from my classes. Until, at one point, I had to take a break from school, and my hospital visits became quite cyclical, and we sought steps separately for something else, a better life somehow.
Jimi: I was diagnosed right at birth, but I didn't find out about my disease until I was a toddler. I remember not being in school and not being able to keep up with my friends in playing soccer, and often needing water breaks. I became sick of it, and one day I went home, and I asked my mom, and that's when she broke the news to me that I had this disease called sickle cell anemia.
I was disappointed because I knew that life seemed extra hard for me as a young toddler. It got me thinking about how life would be for me as a grown man if it were already impacting my life this much as a child. So, when I heard about the disease, I felt bleak.
Jimi: As I grew up, it became increasingly difficult to manage the crises. As a young man, I remember living in Nigeria and having no access to the emergency room and high-powered narcotics. I remember how painful those crises would feel; sometimes, I would pass out from pain and wake up the next morning. It just got worse growing up. Eventually, I moved to the US because I was born here, and we wanted to take advantage of the educational and healthcare system.
I remember my first crisis in the US, going to the emergency room and just being so in awe of how quickly a high-powered medication could alleviate my pain.
I remember coming here to the US excited and ambitious about what I would do and then just having to withdraw every semester from my classes. Until, at one point, I had to take a break from school, and my hospital visits became quite cyclical, and we sought steps separately for something else, a better life somehow.

Managing Sickle Cell Disease as an Adult
Patients may sometimes find it extremely challenging to cope with their constantly recurring symptoms and pain crises. It impacts every aspect of their lives, including access to quality education and professional training and the availability of employment opportunities. Additionally, working through the healthcare system and standard of care processes can sometimes be a nightmare for patients who require immediate attention. In this section, Jimi opens up about his life experiences as an adult and how the disease took a toll on his life while impacting his career and family.
Kevin: Growing into adulthood, how did the condition continue to affect you and your career before your treatment?Jimi: As an adult, it was worse. When I was a pediatric patient, I had the fantastic white-glove care pediatricians usually give children. But as soon as I turned 21, I fell into the traps of adult care.
Every time I went into this abyss of nothingness, where I felt doctors didn't believe me, it was hard to get my pain under control, and it was hard to find a hematologist that would take me seriously.
So, it definitely affected my schooling and then, eventually, my career because I knew that no one was going to hire someone that would show up very little to the office. I knew that I had to find a solution for myself, and that's when my wife and I decided that maybe I should go down the path of being my own boss. Fortunately, I had parents that are business-oriented, so it wasn't a hard step for me to take. I just wish that I had the chance to train myself more.
Jimi: As an adult, it was worse. When I was a pediatric patient, I had the fantastic white-glove care pediatricians usually give children. But as soon as I turned 21, I fell into the traps of adult care.
Every time I went into this abyss of nothingness, where I felt doctors didn't believe me, it was hard to get my pain under control, and it was hard to find a hematologist that would take me seriously.
So, it definitely affected my schooling and then, eventually, my career because I knew that no one was going to hire someone that would show up very little to the office. I knew that I had to find a solution for myself, and that's when my wife and I decided that maybe I should go down the path of being my own boss. Fortunately, I had parents that are business-oriented, so it wasn't a hard step for me to take. I just wish that I had the chance to train myself more.
Minu: It seems the treatment available to you was majorly pain management, is that correct?Jimi: At one point, I did start hydroxyurea, which is very mild chemotherapy. It was initially used for leukemia patients, but they found out that it can help increase fetal hemoglobin levels. I tried that twice but didn't have much success with it, so I stopped. But that and pain management was basically how I managed the disease.
Jimi: At one point, I did start hydroxyurea, which is very mild chemotherapy. It was initially used for leukemia patients, but they found out that it can help increase fetal hemoglobin levels. I tried that twice but didn't have much success with it, so I stopped. But that and pain management was basically how I managed the disease.
Sickle Cell Disease in the African American Community
Sickle cell disease is frequently seen in individuals of African descent. It is estimated that the disease occurs in 1 in every 365 Black or African American births (CDC data). The comprehensive care for sickle cell patients is inferior to that available for other genetic disorders such as hemophilia and cystic fibrosis. Since it was first described nearly 100 years ago, inadequate research has prolonged delays in therapeutic development. Some physicians (partly) attribute this to structural racism and lack of access to education and healthcare facilities within the Black communities. Jimi shares his insights on this aspect through his experiences.
Minu: Sickle cell disease affects Black people more disproportionately. Have you experienced any additional hurdles in getting the right treatment?Jimi: Yeah, because the disease predominantly affects African Americans, unfortunately, it is stigmatized. As an adult, I found that the urgency to take care of me whenever I would go to the emergency room was never really there. I guess this is also because of the standard of care processes. I would just sit and wait for hours to get any attention from a healthcare provider.
I even remember one time being in such severe pain that my wife rushed me to the hospital, and we waited in the lobby for hours. By the time I was able to be seen by a physician, my crisis had already subsided! So yeah, because the disease predominantly affects people of color, there's a lot of stigma.
Jimi: Yeah, because the disease predominantly affects African Americans, unfortunately, it is stigmatized. As an adult, I found that the urgency to take care of me whenever I would go to the emergency room was never really there. I guess this is also because of the standard of care processes. I would just sit and wait for hours to get any attention from a healthcare provider.
I even remember one time being in such severe pain that my wife rushed me to the hospital, and we waited in the lobby for hours. By the time I was able to be seen by a physician, my crisis had already subsided! So yeah, because the disease predominantly affects people of color, there's a lot of stigma.
New Clinical Trials Over the Horizon: Gene Therapy for Sickle Cell Disease
The recent clinical trial CTX001 (CLIMB SCD-121) involved CRISPR targeting to modify fetal hemoglobin expression. The study was funded by CRISPR Therapeutics and Vertex Pharmaceuticals. Fetal hemoglobin is present in all humans during fetal development (in utero), and its expression is turned off at birth. As part of the trial mentioned above, gene editing enabled physicians to turn on fetal hemoglobin production in sickle cell patients. In this section, Jimi talks about the multiple options available to him for long-term treatment and how he focused on the gene therapy trial.
Kevin: Tell us a little more about how you learned about the clinical trials for sickle cell therapy?Jimi: So five or six years ago, the disease was really taking hold of my life. My family encouraged me to find a long-term solution to this. So they encouraged me to do a bone marrow transplant, and my sisters tested to see if there'll be a match for me, but they weren’t. We also saw this other cool thing for which one might not need a full match, and we started exploring stem cell transplants. During my research, I was focused on the recovery time and how long I'll have to take an absence from my life to pursue these therapies, and it just wasn't adding up. I kept on looking, and one day, I came across gene editing, and I was excited about it.
About two years later, I got this NPR article alert about a gene editing trial here in the US, they had tried it on a person, and it seemed to be working in her favor.
Jimi: So five or six years ago, the disease was really taking hold of my life. My family encouraged me to find a long-term solution to this. So they encouraged me to do a bone marrow transplant, and my sisters tested to see if there'll be a match for me, but they weren’t. We also saw this other cool thing for which one might not need a full match, and we started exploring stem cell transplants. During my research, I was focused on the recovery time and how long I'll have to take an absence from my life to pursue these therapies, and it just wasn't adding up. I kept on looking, and one day, I came across gene editing, and I was excited about it.
About two years later, I got this NPR article alert about a gene editing trial here in the US, they had tried it on a person, and it seemed to be working in her favor.

Jimi: My wife was the one who actually reached out, and the next day, Dr. Frangoul, the head researcher for the trial, reached back out to us. He had a brief conversation with me, wanted to make sure I qualified, and they flew us out to Nashville, where the trial would occur. So they flew me out in January 2019 to start the process, which I think took about a whole year.
While we are in utero, we all produce fetal hemoglobin. As soon as we're delivered, our DNA turns off that allele that produces fetal hemoglobin. The gene editing allows to go back and target the allele that is turned off at birth and turn it back on. So, I'm producing fetal hemoglobin nonstop now, and I have more fetal hemoglobin that overwhelms the sickle cell hemoglobin in my system, which makes the symptoms of the disease a lot milder.
Minu: How was the entire experience of participating in such a trial?Jimi: Yeah, it was a little difficult. Before I turned 36 or 35 when I participated in this trial, I would say I spent 20% of my life in hospitals. So that's why I did not want anything that was long-standing where I had to be in a hospital for too long. Even though it wasn't as long as a traditional transplant, I think from when they had collected my DNA and when they manufactured the cells to when I was being conditioned and after the transplant, I probably ended up staying for about three months in the hospital and in a medical apartment before they were able to release me finally.
Jimi: Yeah, it was a little difficult. Before I turned 36 or 35 when I participated in this trial, I would say I spent 20% of my life in hospitals. So that's why I did not want anything that was long-standing where I had to be in a hospital for too long. Even though it wasn't as long as a traditional transplant, I think from when they had collected my DNA and when they manufactured the cells to when I was being conditioned and after the transplant, I probably ended up staying for about three months in the hospital and in a medical apartment before they were able to release me finally.
Recovery After the Transplant and Optimism For the Future
Kevin: How are you doing now after the therapy?Jimi: It has improved drastically. I can do things now that I couldn't even dream of doing before. Before, it used to take me about two weeks to recover from traveling. I would travel and my ankles will swell up so bad that I wouldn't be able to walk and now I don't need that time to recover. Cold weather was something I needed to desperately stay away from because it'll put me into a crisis rather quickly. Now, when we get the rare snowfall here in Atlanta, I can go out and show my son what snow feels like. So it's a lot better.
Jimi: It has improved drastically. I can do things now that I couldn't even dream of doing before. Before, it used to take me about two weeks to recover from traveling. I would travel and my ankles will swell up so bad that I wouldn't be able to walk and now I don't need that time to recover. Cold weather was something I needed to desperately stay away from because it'll put me into a crisis rather quickly. Now, when we get the rare snowfall here in Atlanta, I can go out and show my son what snow feels like. So it's a lot better.

Kevin: Is there continued treatment? Are you still being monitored? Are there any side effects or concerns post-therapy?Jimi: Yeah. So they're going to be watching me for 15 years. So right now, I go back to Nashville every quarter, and it's easier now. Right after the transplant, I think I had to go back every month. But the more distance we put on the post-transplant date, the fewer my checkups are.
No concerns. If anything, it has just been positively overwhelming. I still have the disease, but just because I have so much more fetal hemoglobin flowing in my blood veins, I don't get the crises and the pain like I used to in the past. My blood counts have risen to levels that are better than my family now, so it's pretty cool.
Jimi: Yeah. So they're going to be watching me for 15 years. So right now, I go back to Nashville every quarter, and it's easier now. Right after the transplant, I think I had to go back every month. But the more distance we put on the post-transplant date, the fewer my checkups are.
No concerns. If anything, it has just been positively overwhelming. I still have the disease, but just because I have so much more fetal hemoglobin flowing in my blood veins, I don't get the crises and the pain like I used to in the past. My blood counts have risen to levels that are better than my family now, so it's pretty cool.
Advocating For Sickle Cell Disease Patients: A Word of Advice
Kevin: You mentioned you spend a lot of your time doing speaking engagements. Is there anything you'd like to share with us about those important efforts?Jimi: Yeah, in a way my advocacy has evolved. I used to do a lot of stuff pretransplant as well, blood drives, giving back by donating money to specific charities, creating content to talk about the disease, and so on. But now, I'm slowly evolving my advocacy because there are so many more soldiers that have come and are doing better jobs than I had been able to do in terms of creating awareness for what's going on in the sickle cell community. Now, what I just try to do is try to be as open as possible about my story, and let people know what it's like to live with sickle cell disease.
Mostly now, what I'm doing is mentoring children, specifically here at the Children's Hospital, Atlanta. But yeah, that's typically what I do these days is making sure I'm telling my story as honestly as possible and mentoring when I can.
Jimi: Yeah, in a way my advocacy has evolved. I used to do a lot of stuff pretransplant as well, blood drives, giving back by donating money to specific charities, creating content to talk about the disease, and so on. But now, I'm slowly evolving my advocacy because there are so many more soldiers that have come and are doing better jobs than I had been able to do in terms of creating awareness for what's going on in the sickle cell community. Now, what I just try to do is try to be as open as possible about my story, and let people know what it's like to live with sickle cell disease.
Mostly now, what I'm doing is mentoring children, specifically here at the Children's Hospital, Atlanta. But yeah, that's typically what I do these days is making sure I'm telling my story as honestly as possible and mentoring when I can.
Minu: So is there any advice that you would give to others who are maybe suffering from this disease, looking for therapies?Jimi: Well, advice is usually tough because everyone's situation is different. I mean, I was in a position to take a year off my life to have this treatment. To be fair, I had done the analysis and I actually thought that it would have to be riskier for me not to do this transplant than if I just continued going on with life because I was becoming a father, that's actually what pushed me to do it. So it's always hard to give advice but one thing I would say is if anyone is considering a CRISPR gene editing trial or any trial, I definitely think they should give it a serious look, and do some research. There are more stories out there like mine that people that have done this trial and they can see the positive effects of it.
Usually, words fail, the advice most people get just hangs in there, wait, there's light at the end of the tunnel. But this time it's real, there is actually light at the end of the tunnel. Now there's something that's tangible and God willing one day, this would be available widely to consumers everywhere. So, if anyone's suffering from a chronic illness, this can potentially help.
There are also other treatments coming out specifically for sickle cell disease and different medications that the FDA is approving. If gene editing is too scary for you, there are other options for you out there with other medications. So, three cheers for modern medicine, I'm just really happy that technology is taking us to a place where people don't have to live with a disease like sickle cell anymore.
Jimi: Well, advice is usually tough because everyone's situation is different. I mean, I was in a position to take a year off my life to have this treatment. To be fair, I had done the analysis and I actually thought that it would have to be riskier for me not to do this transplant than if I just continued going on with life because I was becoming a father, that's actually what pushed me to do it. So it's always hard to give advice but one thing I would say is if anyone is considering a CRISPR gene editing trial or any trial, I definitely think they should give it a serious look, and do some research. There are more stories out there like mine that people that have done this trial and they can see the positive effects of it.
Usually, words fail, the advice most people get just hangs in there, wait, there's light at the end of the tunnel. But this time it's real, there is actually light at the end of the tunnel. Now there's something that's tangible and God willing one day, this would be available widely to consumers everywhere. So, if anyone's suffering from a chronic illness, this can potentially help.
There are also other treatments coming out specifically for sickle cell disease and different medications that the FDA is approving. If gene editing is too scary for you, there are other options for you out there with other medications. So, three cheers for modern medicine, I'm just really happy that technology is taking us to a place where people don't have to live with a disease like sickle cell anymore.
Other CRISPR and Gene Therapy Podcasts You May Enjoy
If you’re looking for new podcasts about genome engineering and personalized medicine, and enjoyed listening to this podcast, here’s a list that you may be interested in:
The Promising Potential of CRISPR Editing in Stem Cells: A Chat with Bill SkarnesCRISPR has simplified gene editing in stem cells, thus showing promising potential in therapy development. In this podcast episode, Dr. Bill Skarnes from the Jackson Laboratory elaborates on how CRISPR-edited stem cells are transforming disease modeling studies.
Full episode here
CRISPR has simplified gene editing in stem cells, thus showing promising potential in therapy development. In this podcast episode, Dr. Bill Skarnes from the Jackson Laboratory elaborates on how CRISPR-edited stem cells are transforming disease modeling studies.
Full episode here
Improving Targeted Delivery to Enhance Personalized MedicineIn this episode we chat with Andre Watson, CEO, and co-founder of Ligandal, a company working to make gene therapy real. They focus on improving the payload delivery of these therapies - something that hasn’t been a real focus of developing CRISPR applications and creates a bottleneck for many amazing new technologies.
Full episode here
In this episode we chat with Andre Watson, CEO, and co-founder of Ligandal, a company working to make gene therapy real. They focus on improving the payload delivery of these therapies - something that hasn’t been a real focus of developing CRISPR applications and creates a bottleneck for many amazing new technologies.
Full episode here
Bryce Olson Relays His Experience on Personalized Therapies for Cancer PatientsAfter being diagnosed with aggressive prostate cancer, Bryce Olson quickly learned the science behind it and has leveraged NGS to understand his tumor genomics and find opportunities in personalized therapies. Hear the patient perspective for the first time on our podcast through Bryce's narration of his experience and pursuit of next-generation cell and gene therapies.
Full episode here
After being diagnosed with aggressive prostate cancer, Bryce Olson quickly learned the science behind it and has leveraged NGS to understand his tumor genomics and find opportunities in personalized therapies. Hear the patient perspective for the first time on our podcast through Bryce's narration of his experience and pursuit of next-generation cell and gene therapies.
Full episode here
Avery Posey Discusses CAR T Cell Cancer TherapiesDr. Avery Posey, Jr. is leading the charge on CAR T cell therapy research and working towards bringing this technology to cancer patients as soon as possible. In this episode, he explains how CAR T works, what stage it’s in now, and how it will help revolutionize the treatment of cancer.
Full episode here
Dr. Avery Posey, Jr. is leading the charge on CAR T cell therapy research and working towards bringing this technology to cancer patients as soon as possible. In this episode, he explains how CAR T works, what stage it’s in now, and how it will help revolutionize the treatment of cancer.
Full episode here