Contents
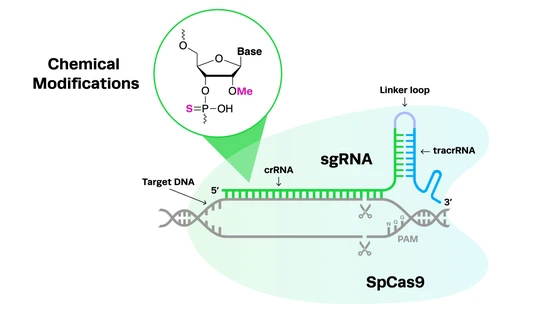
CRISPR-Cas9 is a groundbreaking technology that was first described in bacteria. Once researchers realized that genes could be precisely edited in any organism, it opened up new avenues for CRISPR applications. This genome engineering tool has particularly made a splash in therapeutics, and is quickly changing the way scientists think about treating genetic disorders.
Mouse Models: First Step in New Disease Therapies
CRISPR clinical trials are on the horizon for several diseases, and even underway for few diseases. But before ever reaching the public, any new therapy is tested exhaustively in the laboratory to ensure complete safety and efficacy. The early stages of laboratory research begin by using animals models to test hypotheses and potential new drugs. While CRISPR has made it relatively simpler to genetically edit complex animals, rodent models (typically mice) are commonly used to model human disease due to their high homology with the human genome.
Manipulation of the mouse genome has and continues to provide scientists with answers to many diseases plaguing our population today. Mouse models with specific silencing or mutation events are oftentimes used to study specific cancers, such as Kras in pancreatic cancer or Apc in colorectal cancer. Additionally,
mouse models of Alzheimer’s disease are used to understand disease manifestation and potential therapies. One of the commonly studied disease groups that have contributed to developing potential novel therapeutics includes inherited blindness and vision disorders.
Gene Insertion Restores Vision in Blind Mice
A very recent study, published in March 2019 in Nature Communications, has been in the news for a successful gene therapy that restored vision in mice suffering from retinal degeneration. In this study, researchers from the University of California, Berkeley, used an adeno-associated virus (AAV) carrying the gene encoding a medium-wavelength light-sensitive receptor and injected it into mice. The AAV essentially acts as a delivery system of genetic material to where scientists want it to act. Following injection, researchers found that in the blind mice, the normally light-insensitive cells began to respond and send signals to the brain interpreted as light. As validation, the mice were subjected to a number of tests including distinguishing differences in line spacing, thickness, and movement. The researchers noted that the treated mice performed similarly to wild-type mice in these tests.
Although this study did not formally use CRISPR in their experiments, their use of gene therapy highlights how scientists are looking to treat blindness. Continuing research efforts and advancements are being made in this field, and CRISPR is playing a huge role in making that happen.
CRISPR Knockout Mice Are Able to Reverse Blindness
The editing strategy behind CRISPR-Cas technology involves cutting of DNA at a target site to generate knockouts or knock-ins. Both CRISPR knockout and CRISPR knock-in mechanisms have been used in mouse models of disease. In the CRISPR knockout model, non-homologous end joining (NHEJ) repairs DNA by filling in nucleotides at the break site causing frameshift mutations that silence the gene. This CRISPR knockout strategy has been used to reverse blindness in mice. Yu et al. used AAV-mediated CRISPR-Cas9 to target the knockout a specific gene in order to improve the survival of a subset of cells in the eye in order to preserve function and vision. Loss of gene expression in these cells resulted in changes in their inherent characteristics that ultimately increased their probability of survival.
CRISPR Knock-in Mice: Ablate & Replace Strategy
The second way to repair DNA is called homology-directed repair (HDR), often referred to as a knock-in strategy. In HDR, a user-defined repair template composed of specific sequences is inserted where the cut was made. Although knock-ins are classically more difficult than knockouts, they are also being used in mouse models to study diseases such as blindness.
For example, researchers have used CRISPR knock-ins in a mouse model of retinitis pigmentosa (RP) to test whether they can reverse blindness in mice. RP is a genetic disorder that causes dysfunction or loss of cells in the retina, oftentimes leading to difficulty and/or loss of vision. RP can be attributed to a single mutation in one of more than 50 genes. Dr. Stephen H. Tsang and his group used an “ablate-and-replace” strategy to knock out a gene involved in RP using CRISPR and replaced it with a wild-type (or non-mutated version) of the gene using exogenous cDNA.
CRISPR Shows Promise in Other Diseases in Mice
Researchers are working hard to develop and test novel ways to use CRISPR to help edit out mutations or typos in our genetic code that lead to disease. The initial studies described in this article using CRISPR to reverse the effects of retinal degeneration and RP showcase the power CRISPR has as a potential “eraser” of inherited disorders.
Overall, researchers are providing much-needed hope for those affected by genetic mutations that can benefit from CRISPR treatment. For instance, the approach of using CRISPR-Cas9 to edit the ß-globin gene to increase fetal hemoglobin levels has been shown to successfully correct sickle-cell disease in mice. CRISPR-Cas9 is also showing
promising results in editing the genetic allele responsible for Huntington’s disease. In Alzheimer’s disease, researchers are using CRISPR-Cas9 to disrupt the gene involved in increasing levels of amyloid-ß protein. Successful editing and consequently lowering of the amyloid ß-protein may help protect against early-onset Alzheimer’s disease.
Promising results from studies using CRISPR in mouse models are helping researchers bring CRISPR closer into the clinic, where the ultimate goal is to help address the need for new therapeutics for human diseases. The success of these and future studies will hopefully translate to more clinical trials and eventually gene and cell-based therapies in the next few years.