Contents
Recent applications of CRISPR genome engineering have made incredible strides, especially in the field of medicine. With amazing developments in healthcare, such as CRISPR CAR T therapy, now more than ever, the diseases that pose the greatest challenge to medical professionals could be a problem of the past.
In this episode of the CRISPR Cuts podcast, we sat down with Andre Watson, CEO and co-founder of Ligandal, a company working to make gene therapy real. They focus on improving the payload delivery of these therapies - something that hasn’t been a real focus of developing CRISPR applications, and creates a bottleneck for many amazing new technologies.
Listen to the podcast on iTunes, or read on to get the gist of the conversation. To start you off, here are some of the most important points made by Watson in the podcast.
5 Key Takeaways in this Podcast About Gene Delivery
In this podcast, Andre Watson of Ligandal shares insight on some cutting-edge developments in the world of gene editing. Here are the main points you’d be sorry to miss.
1. Gene therapy companies focus on developing, not deliveringOnce CRISPR was popularized, gene therapy companies focused on developing therapies because they knew it would be so important, but the technology required to target specific cells had not caught up, so there really wasn’t any way to get them to market.
Time in podcast: 4:45
Once CRISPR was popularized, gene therapy companies focused on developing therapies because they knew it would be so important, but the technology required to target specific cells had not caught up, so there really wasn’t any way to get them to market.
Time in podcast: 4:45
2. Though cell delivery is currently tailored to specific types of cells, this will changeLigandal is working to create delivery that could be uniform for various types of cells, helping improve on current methods that can only target specific types of cells.
Time in podcast: 8:00
Ligandal is working to create delivery that could be uniform for various types of cells, helping improve on current methods that can only target specific types of cells.
Time in podcast: 8:00
3. Computational tools will improve the science of gene editingLigandal has developed a method that is improved over time with computational tools. They are recognizing patterns that could reduce the time of some gene editing processes that typically take months to days - or even as little as hours.
Time in podcast: 11:50
Ligandal has developed a method that is improved over time with computational tools. They are recognizing patterns that could reduce the time of some gene editing processes that typically take months to days - or even as little as hours.
Time in podcast: 11:50
4. Personalized gene immuno-oncology is nearSoon, treatments like CAR T-cell therapy will revolutionize cancer treatment, and the treatment of other complex diseases like sickle cell anemia or beta thalassemia.
Time in podcast: 15:00
Soon, treatments like CAR T-cell therapy will revolutionize cancer treatment, and the treatment of other complex diseases like sickle cell anemia or beta thalassemia.
Time in podcast: 15:00
5. Soon, gene therapy targeting will be so advanced, we will treat diseases like never before
For example, if a patient had Alzheimer’s disease, and we know the cause of that is related to old age, there may be therapies available to treat the gene that causes the aging process to happen preemptively.
Time in podcast: 18:20
For example, if a patient had Alzheimer’s disease, and we know the cause of that is related to old age, there may be therapies available to treat the gene that causes the aging process to happen preemptively.
Time in podcast: 18:20
Andre Watson’s Background and Story
Get insight into how Andre Watson went from his undergrad at Rensselaer Polytechnic Institute (RPI) in New York to founding one of the most cutting-edge gene therapy companies currently out there.
Minu: Let's begin this episode by talking a little bit about your educational background.Andre: Sure. I was studying Biomedical Engineering at RPI when I decided that gene delivery was this big missing piece within medicine. So we had all these tools for sequencing the genome, for understanding what causes various diseases, and yet even with the advance of tools like CRISPR, there weren't effective ways of actually reprogramming that molecular information to rid the body of negative pathology.
I became fascinated with the idea of how you could actually deliver genetic cargo and different genetic engineering tools to the appropriate places in the body, and create a platform for targeting specific cells. I spent two years during my undergrad building what ended up being the first proof of concept for delivering a guided nuclease, which is CRISPR, into targeted cells, without using a virus.
Andre: So the first work really centered around delivering TALENs, which were kind of a precursor to CRISPR, and were still quite a good gene editing tool. We did a series of studies all the way to in vivo mouse studies, where we injected adult mice with a bone fragility disease, with the gene editing constructs carried by these nanoparticles, into their bone marrow.
Around 2013, I took it to Silicon Valley, and it was really a choice between do I go get my Ph.D., spend another six years in academia, or do I take the data and intellectual property and use the knowledge that I have in this burgeoning industry and create a missing piece for delivery. So, we've been working on creating iterative delivery systems for the last five years at Ligandal.
Minu: So that's how you ended up founding Ligandal after your undergrad, just deciding not to continue in academia anymore. That's a big step going from undergrad right into a company. But I guess the interesting part here is really the technique which you developed or proof of concept which you developed during your undergrad studies.
Andre: Sure. I was studying Biomedical Engineering at RPI when I decided that gene delivery was this big missing piece within medicine. So we had all these tools for sequencing the genome, for understanding what causes various diseases, and yet even with the advance of tools like CRISPR, there weren't effective ways of actually reprogramming that molecular information to rid the body of negative pathology.
I became fascinated with the idea of how you could actually deliver genetic cargo and different genetic engineering tools to the appropriate places in the body, and create a platform for targeting specific cells. I spent two years during my undergrad building what ended up being the first proof of concept for delivering a guided nuclease, which is CRISPR, into targeted cells, without using a virus.
Andre: So the first work really centered around delivering TALENs, which were kind of a precursor to CRISPR, and were still quite a good gene editing tool. We did a series of studies all the way to in vivo mouse studies, where we injected adult mice with a bone fragility disease, with the gene editing constructs carried by these nanoparticles, into their bone marrow.
Around 2013, I took it to Silicon Valley, and it was really a choice between do I go get my Ph.D., spend another six years in academia, or do I take the data and intellectual property and use the knowledge that I have in this burgeoning industry and create a missing piece for delivery. So, we've been working on creating iterative delivery systems for the last five years at Ligandal.
Minu: So that's how you ended up founding Ligandal after your undergrad, just deciding not to continue in academia anymore. That's a big step going from undergrad right into a company. But I guess the interesting part here is really the technique which you developed or proof of concept which you developed during your undergrad studies.
Why CRISPR Companies Can’t Succeed Without Better Targeted Gene Delivery Systems
Many gene therapy companies have done amazing work in the past few years, but are still waiting on the technology of targeted gene delivery. Learn what has happened thus far, and what scientific developments still need to happen.
Minu: Ligandal focuses on unique delivery of gene therapies, so the first question then would be why do we have a delivery problem? Maybe you could elaborate on why we had this gap that needed to be filled.
Andre: Well, going back to even the 1970s, you had all kinds of chemotherapy drugs like Docetaxel and Paclitaxel, and at some point, it was discovered that you package out the chemotherapy agents into nanoparticles, and make them more efficient.
You could now dose a patient with less chemo drug or the same amount of chemo drug, but it would distribute to the cancerous tissue better. The problem that didn't get solved is creating delivery systems that actually target the specific cells and tissues and can bear any number of payloads. So for the longest time, delivery systems were these kind of ‘passive materials’ that would package up what we want delivered and you'd just put it in the blood and look at where it's distributing.
But the materials themselves weren't necessarily smart. And when I say smart, I mean able to target a specific cell - or in the case of delivering a genetic construct, also able to get into the nucleus of the cells. So we need both of these pieces, and we have many barriers and many stages that you need to get past; you need it to survive in the blood, and you need to get the target itself to each of those constructs, and then you need to protect the delicate genetic payloads until they reach the desired location.
Clearly, there are many places where things can go wrong. One thing that we found was that there were a lot of these companies focusing on gene editing, even dating back to the late 90s with Sangamo, Cellectis, and Precision Biosciences. Now we have all these CRISPR companies like Editas, Intellia, CRISPR Therapeutics, but these companies all continue to put the payload first. So in other words you have CRISPR, you form a company, and then you figure out okay, where can I get CRISPR to? Where's the industry capable of delivering it?
People end up sort of reusing and recycling different delivery systems that have been used for a number of years, without actually focusing on the core advancement of delivery. Which has resulted in very limited addressable tissue and cellular targets. In other words, if you want to deliver something to the liver, that's easy. We've been able to deliver things to the liver for a very long time. But if you want to target a specific cell in your blood or target a specific cell in your pancreas, that sort of work has only been more recent when it's dealing with genetic constructs.
There was this opportunity in 2013 when I moved out here, when none of the CRISPR companies had formed yet. So we didn't have Editas, we didn't have these other companies, we just had the first initial papers. And at the time, if you actually Googled gene editing nanoparticles back in 2013, there were two results, and they were getting sub-one percent efficiency and they weren't even using CRISPR. So really that was the opportunity. The opportunity came from this rapid advancement in the number of publications and the number of companies trying to do gene editing. But no one was focusing on how to actually deliver those constructs.
And it was just assumed that if you put enough money into a CRISPR company, they'll just figure it out. Well, it's been five years. And in that time, it hasn't been figured out. So once again, you can get to the liver, you can inject something into the back of the eye, you can put stuff on some cells in a dish. But when it comes to actually saying I want to reprogram this specific cell or tissue in this specific organ using a specific construct, that is a very long intensive process.
And at this point, I was just at a JP Morgan meeting with a number of gene editing companies and immunotherapy companies and so on, and I keep hearing that there's really this critical bottleneck, even today, in terms of developing the vectors for delivery. Such that if you actually want to go out and have a virus designed or use in a dish for your T-cell immunotherapy or whatever you're developing, it's going to take you a minimum of 12 months just to get past the backlog and the waiting period for one of the handful of companies that actually can develop these viruses for you, and then another six months to manufacture, at least.
So, there is a huge demand for delivery systems, but the supply isn't there. So if you can create cost effective delivery systems that are non-viral, that can target specific cells and deliver a range of constructs, you're creating a lot of value for your industry at large, and in turn, creating very valuable therapeutics if you could get them to market.
Andre: Well, going back to even the 1970s, you had all kinds of chemotherapy drugs like Docetaxel and Paclitaxel, and at some point, it was discovered that you package out the chemotherapy agents into nanoparticles, and make them more efficient.
You could now dose a patient with less chemo drug or the same amount of chemo drug, but it would distribute to the cancerous tissue better. The problem that didn't get solved is creating delivery systems that actually target the specific cells and tissues and can bear any number of payloads. So for the longest time, delivery systems were these kind of ‘passive materials’ that would package up what we want delivered and you'd just put it in the blood and look at where it's distributing.
But the materials themselves weren't necessarily smart. And when I say smart, I mean able to target a specific cell - or in the case of delivering a genetic construct, also able to get into the nucleus of the cells. So we need both of these pieces, and we have many barriers and many stages that you need to get past; you need it to survive in the blood, and you need to get the target itself to each of those constructs, and then you need to protect the delicate genetic payloads until they reach the desired location.
Clearly, there are many places where things can go wrong. One thing that we found was that there were a lot of these companies focusing on gene editing, even dating back to the late 90s with Sangamo, Cellectis, and Precision Biosciences. Now we have all these CRISPR companies like Editas, Intellia, CRISPR Therapeutics, but these companies all continue to put the payload first. So in other words you have CRISPR, you form a company, and then you figure out okay, where can I get CRISPR to? Where's the industry capable of delivering it?
People end up sort of reusing and recycling different delivery systems that have been used for a number of years, without actually focusing on the core advancement of delivery. Which has resulted in very limited addressable tissue and cellular targets. In other words, if you want to deliver something to the liver, that's easy. We've been able to deliver things to the liver for a very long time. But if you want to target a specific cell in your blood or target a specific cell in your pancreas, that sort of work has only been more recent when it's dealing with genetic constructs.
There was this opportunity in 2013 when I moved out here, when none of the CRISPR companies had formed yet. So we didn't have Editas, we didn't have these other companies, we just had the first initial papers. And at the time, if you actually Googled gene editing nanoparticles back in 2013, there were two results, and they were getting sub-one percent efficiency and they weren't even using CRISPR. So really that was the opportunity. The opportunity came from this rapid advancement in the number of publications and the number of companies trying to do gene editing. But no one was focusing on how to actually deliver those constructs.
And it was just assumed that if you put enough money into a CRISPR company, they'll just figure it out. Well, it's been five years. And in that time, it hasn't been figured out. So once again, you can get to the liver, you can inject something into the back of the eye, you can put stuff on some cells in a dish. But when it comes to actually saying I want to reprogram this specific cell or tissue in this specific organ using a specific construct, that is a very long intensive process.
And at this point, I was just at a JP Morgan meeting with a number of gene editing companies and immunotherapy companies and so on, and I keep hearing that there's really this critical bottleneck, even today, in terms of developing the vectors for delivery. Such that if you actually want to go out and have a virus designed or use in a dish for your T-cell immunotherapy or whatever you're developing, it's going to take you a minimum of 12 months just to get past the backlog and the waiting period for one of the handful of companies that actually can develop these viruses for you, and then another six months to manufacture, at least.
So, there is a huge demand for delivery systems, but the supply isn't there. So if you can create cost effective delivery systems that are non-viral, that can target specific cells and deliver a range of constructs, you're creating a lot of value for your industry at large, and in turn, creating very valuable therapeutics if you could get them to market.
How Ligandal is Changing Gene Payload Delivery
Ligandal chose instead to focus on delivering gene therapies into the body with precision and efficiency. Learn about the science behind their method, and why no one else is doing this?
Minu: That's very interesting and makes a lot of sense to think about how these gene therapies would even get into the body. Now, one question that I had was that with ligands, which will specifically bind to receptors on particular type of cells - which is a very smart way to get into a particular type of cell.
However, this also means that every therapy would have to be tailored, and it cannot be a general platform which can be used for all kinds of therapies, right? So is the bottleneck for you right now to basically figure out and establish great delivery methods for each type of cell? Or is there a way to make it uniform for any type of cell?Andre: Well, that's exactly what we've really developed at Ligandal. The idea is that anytime you have a cell, it's going to have a certain profile of receptors, so, we have two pieces to really develop in our platform. One is knowing that you can actually package up a given payload. The second is knowing that you can actually get that payload to the target itself. So we develop both of those things. We create an iterative process to take a range of polymers that are actually based on peptides, and condense them around the given payload they want to deliver, such as CRISPR, so that you form a stable package.
Then we decorate that package in targeting ligands, and we have a discovery platform for really rapidly creating ligands. So we can take an unspecified cell, and based on the knowledge of which receptors it has, we can create targeting molecules, targeting ligands, faster than anyone else. We've created an advancement not just in the delivery system and the packaging, but also in the targeting and being able to create ligands in hours or days, instead of months.
Andre: Well, that's exactly what we've really developed at Ligandal. The idea is that anytime you have a cell, it's going to have a certain profile of receptors, so, we have two pieces to really develop in our platform. One is knowing that you can actually package up a given payload. The second is knowing that you can actually get that payload to the target itself. So we develop both of those things. We create an iterative process to take a range of polymers that are actually based on peptides, and condense them around the given payload they want to deliver, such as CRISPR, so that you form a stable package.
Then we decorate that package in targeting ligands, and we have a discovery platform for really rapidly creating ligands. So we can take an unspecified cell, and based on the knowledge of which receptors it has, we can create targeting molecules, targeting ligands, faster than anyone else. We've created an advancement not just in the delivery system and the packaging, but also in the targeting and being able to create ligands in hours or days, instead of months.
Minu: I see. That's excellent actually. And correct me if I'm wrong, but Ligandal is the first company to basically use these kind of cell specific biomolecules for targeting a gene or gene material inside those, right?
Andre: Exactly. And we're basing these ligands entirely off human-derived proteins. We're using biology to interact with biology, rather than trying to discover things from scratch.
Andre: Exactly. And we're basing these ligands entirely off human-derived proteins. We're using biology to interact with biology, rather than trying to discover things from scratch.
Minu: Why are other scientists struggling in what you want to achieve, and why aren’t other companies popping up trying to do the same thing, or even managing to do the same thing?
Andre: Well there have been a few companies that have appeared that are trying to do gene editing delivery, and they typically either don't have the targeting component and they're just trying to do local injections, or they're using some form of, for example, an aptamer for targeting cells. And the thing with using aptamers or antibodies is you have to do a lot of screening and a lot of development to get your targeting molecule actually made - then you can stick it onto a nanoparticle.
But the issue with the gene editing and the gene constructs is that you need to actually get them into the nucleus of the cell after you get there, and you need to survive the endosome. So what we've seen, is there's been a lack of innovation in the fundamental delivery systems. A lot of people are trying to use liposomes or lipid nanoparticles that you basically create like a soap bubble with your package inside and then you can decorate it with targeting elements.
But what we're doing is actually screening a much broader array of gene delivery materials than we've seen anyone publish or even talk about.
Andre: Well there have been a few companies that have appeared that are trying to do gene editing delivery, and they typically either don't have the targeting component and they're just trying to do local injections, or they're using some form of, for example, an aptamer for targeting cells. And the thing with using aptamers or antibodies is you have to do a lot of screening and a lot of development to get your targeting molecule actually made - then you can stick it onto a nanoparticle.
But the issue with the gene editing and the gene constructs is that you need to actually get them into the nucleus of the cell after you get there, and you need to survive the endosome. So what we've seen, is there's been a lack of innovation in the fundamental delivery systems. A lot of people are trying to use liposomes or lipid nanoparticles that you basically create like a soap bubble with your package inside and then you can decorate it with targeting elements.
But what we're doing is actually screening a much broader array of gene delivery materials than we've seen anyone publish or even talk about.
How Computational Tools are Helping Advance CRISPR
Learn more about how Ligandal uses computational tools to make their science more precise, and help improve it, and the work of all genome engineering scientists over time.
Minu: You mentioned this before, but recently there has been a huge component of computational biology in any generalized biology platform, which was not the case before. Are computational tools an important part of the work that you do at Ligandal, are they mixing in well with biology now?Andre: The computational component is very important, but it's not all encompassing. One of the great things about the idea of a computational platform is it can simulate a lot of things. But at the end of the day, you're going to have to interact with biological systems which are highly dynamic, complex, and really are more amenable to brute forcing methods of screening. So, you need to find the right balance between simulating things and actually performing the experiments.
That's the balance that we've tried to find at Ligandal, where there is a simulation component, so we do look at creating ligands that haven't been used before. But we're starting from native proteins, so we're not starting completely de novo, trying to make sequences that didn't exist before. That's the first piece.
The second piece is actually making the nanoparticles, and there are many components that go into making a nanoparticle. In our case, we use electrostatic interactions, which are charged interactions between negatively charged things, especially with gene that you're delivering. And positively charged things, such as the peptide sequences that actually package up that payload.
What we actually developed is a software interface for rapidly designing those experiments and having robots perform those experiments. So we tied the computational elements, which are really simulating and designing the targeting molecules, to the physical studies of making nanoparticles. And that is something that also, much like biology, you can't fully predict. So we need to screen hundreds of things, but we end up iterating and finding patterns that work.
And once we lock in those patterns and find the things that are consistent in their formulations for the size of those particles, how well they packaged the materials, etc., we then do a biological study and look at how well those nanoparticles performed in a cellular context. So every time we perform an experiment, we can take the top 10 or 20 percent of performing groups, wipe those out, and then the rest are iterated around. So it continues to get better and better.
That's really the novelty of our approach. We're not just trying to take an off the shelf delivery system, put something inside of it, and hope that it targets the right cell. We're actually tuning and fine tuning all of the aspects of how you'd want to interact with a cell down to the level of what enzyme is going to break apart my nanoparticle. Is it going to go to the nucleus? Is it going to release quickly or slowly? Is it going to be a big particle or a small particle? Is it targeting one receptor or another? All of those things are what we’re looking to nail down.
Andre: The computational component is very important, but it's not all encompassing. One of the great things about the idea of a computational platform is it can simulate a lot of things. But at the end of the day, you're going to have to interact with biological systems which are highly dynamic, complex, and really are more amenable to brute forcing methods of screening. So, you need to find the right balance between simulating things and actually performing the experiments.
That's the balance that we've tried to find at Ligandal, where there is a simulation component, so we do look at creating ligands that haven't been used before. But we're starting from native proteins, so we're not starting completely de novo, trying to make sequences that didn't exist before. That's the first piece.
The second piece is actually making the nanoparticles, and there are many components that go into making a nanoparticle. In our case, we use electrostatic interactions, which are charged interactions between negatively charged things, especially with gene that you're delivering. And positively charged things, such as the peptide sequences that actually package up that payload.
What we actually developed is a software interface for rapidly designing those experiments and having robots perform those experiments. So we tied the computational elements, which are really simulating and designing the targeting molecules, to the physical studies of making nanoparticles. And that is something that also, much like biology, you can't fully predict. So we need to screen hundreds of things, but we end up iterating and finding patterns that work.
And once we lock in those patterns and find the things that are consistent in their formulations for the size of those particles, how well they packaged the materials, etc., we then do a biological study and look at how well those nanoparticles performed in a cellular context. So every time we perform an experiment, we can take the top 10 or 20 percent of performing groups, wipe those out, and then the rest are iterated around. So it continues to get better and better.
That's really the novelty of our approach. We're not just trying to take an off the shelf delivery system, put something inside of it, and hope that it targets the right cell. We're actually tuning and fine tuning all of the aspects of how you'd want to interact with a cell down to the level of what enzyme is going to break apart my nanoparticle. Is it going to go to the nucleus? Is it going to release quickly or slowly? Is it going to be a big particle or a small particle? Is it targeting one receptor or another? All of those things are what we’re looking to nail down.
When Will Personalized Medicine Reach Everyday People?
When will this enhancement help bring targeted gene therapies to real patients? What is currently holding us back?
Minu: There are several steps and optimization cycles until you get to a point where something actually works as well as you want it. So now that you have this platform and you are finding ways in which you can have even more efficient delivery systems, how far are we from personalized medicine? So what is the gap right now?Andre: Well, I think there are different degrees of personalized medicine. I think what we're going to see sooner rather than later, is diagnostically responsive immunotherapy. So taking a T-cell, for example, and reprogramming it to attack a specific kind of cancer cell, because the FDA's already approved the first gene therapy or immuno-oncology, as is Novartis' Kymriah in 2017. We're now looking at an exponential advancement in the field around autologous cell therapies.
So, in this case, you have to take an immune cell, a T-cell, that normally surveys your whole body, and you have this huge variety of these so-called T-cell receptors that each respond to different antigens or different markers that shouldn't belong in your body. So that could be a virus, that could be some sort of bacteria, or it could be cancer that you just developed with its own set of mutations, and results, and new sequences of proteins on the surface.
Our immune system can recognize all of these things. With immunotherapy, the goal in the case of T-cell immunotherapy is to take those T-cells and to give them targeting characteristics, where you genetically engineer the cell so that it can stick to a specific kind of cancer cell or a specific kind of virus.
There are companies now trying to focus on the personalized aspect of that. One of them is called Pact Pharma, for example, where they're actually sequencing your tumor, they're identifying which neoantigens or new peptide sequences that tumor has. And then they're actually building this microfluidic platform where they'll pull out your cells and circulating T cells will go through this chip, and they will stick to those peptide sequences that you identified in that patient.
And the T-cells that get pulled out are the ones that already have recognition for that neoantigen. Then you have the sequence of the T-cells, identify which T-cell receptors they have, and then you have to genetically engineer a larger population of that person's T-cells to have the same sequence.
That's a complex process, but that's kind of the first foray that we're seeing into personalized gene editing immuno-oncology. We're also going to see a lot of stuff in the genetic disease space. So, you have a disease like Sickle cell disease where you have a single base pair that results in the disease. That's a pretty easy off-the-shelf fix, if you can actually deliver to the right cells or even perform in a target cell transplantation.
But then you have diseases like Beta thalassemia or Von Willebrand disease where you have hundreds of different mutations underlying even a single genetic disease. Where, yes, it is the one gene that’s affected, but it can have many, many different mutations that result in the pathology. So how do you treat those diseases? You're going to have to actually stratify patient population within that single disease into different gene editing modalities, if you're going the gene editing route.
And then we have more complex, multi-factorial diseases also. So we're going to be treating the disease of aging itself, where you're going to say that an older person isn't just sick because they have Alzheimer's disease, you're going to say they're sick because they got older, and maybe there's a comprehensive set of things that you need to do to reverse the biological age of the human. So that could take decades to really mature, but as it matures we're looking at actually saying here's a diagnosis, here is the set of genetic changes that I'd like to affect in the patient, whether they are temporary or permanent. And here are the tissues in which I'd like to create those changes.
I think delivery is a bottleneck to being able to do that. Because you can't always do a cell therapy, you can't always just target the liver. You're going to need to actually predictably say I'm going to fix X, Y, Z cells to choose an organ with A, B, C, D, E, F, G, different genetic traits.
Andre: Well, I think there are different degrees of personalized medicine. I think what we're going to see sooner rather than later, is diagnostically responsive immunotherapy. So taking a T-cell, for example, and reprogramming it to attack a specific kind of cancer cell, because the FDA's already approved the first gene therapy or immuno-oncology, as is Novartis' Kymriah in 2017. We're now looking at an exponential advancement in the field around autologous cell therapies.
So, in this case, you have to take an immune cell, a T-cell, that normally surveys your whole body, and you have this huge variety of these so-called T-cell receptors that each respond to different antigens or different markers that shouldn't belong in your body. So that could be a virus, that could be some sort of bacteria, or it could be cancer that you just developed with its own set of mutations, and results, and new sequences of proteins on the surface.
Our immune system can recognize all of these things. With immunotherapy, the goal in the case of T-cell immunotherapy is to take those T-cells and to give them targeting characteristics, where you genetically engineer the cell so that it can stick to a specific kind of cancer cell or a specific kind of virus.
There are companies now trying to focus on the personalized aspect of that. One of them is called Pact Pharma, for example, where they're actually sequencing your tumor, they're identifying which neoantigens or new peptide sequences that tumor has. And then they're actually building this microfluidic platform where they'll pull out your cells and circulating T cells will go through this chip, and they will stick to those peptide sequences that you identified in that patient.
And the T-cells that get pulled out are the ones that already have recognition for that neoantigen. Then you have the sequence of the T-cells, identify which T-cell receptors they have, and then you have to genetically engineer a larger population of that person's T-cells to have the same sequence.
That's a complex process, but that's kind of the first foray that we're seeing into personalized gene editing immuno-oncology. We're also going to see a lot of stuff in the genetic disease space. So, you have a disease like Sickle cell disease where you have a single base pair that results in the disease. That's a pretty easy off-the-shelf fix, if you can actually deliver to the right cells or even perform in a target cell transplantation.
But then you have diseases like Beta thalassemia or Von Willebrand disease where you have hundreds of different mutations underlying even a single genetic disease. Where, yes, it is the one gene that’s affected, but it can have many, many different mutations that result in the pathology. So how do you treat those diseases? You're going to have to actually stratify patient population within that single disease into different gene editing modalities, if you're going the gene editing route.
And then we have more complex, multi-factorial diseases also. So we're going to be treating the disease of aging itself, where you're going to say that an older person isn't just sick because they have Alzheimer's disease, you're going to say they're sick because they got older, and maybe there's a comprehensive set of things that you need to do to reverse the biological age of the human. So that could take decades to really mature, but as it matures we're looking at actually saying here's a diagnosis, here is the set of genetic changes that I'd like to affect in the patient, whether they are temporary or permanent. And here are the tissues in which I'd like to create those changes.
I think delivery is a bottleneck to being able to do that. Because you can't always do a cell therapy, you can't always just target the liver. You're going to need to actually predictably say I'm going to fix X, Y, Z cells to choose an organ with A, B, C, D, E, F, G, different genetic traits.
Minu: So there are types of therapies that you mentioned, for example, T cell therapy. These are ex vivo therapies, that you would take, or at least for now, you would take immune cells from patients and then edit them outside the body, and then reinsert them back into the patient. Would you say that delivery systems are more of a bottleneck or are more critical for in vivo gene therapy?Andre: Well, certainly in vivo is a huge bottleneck. But we're seeing that the bottleneck is even in the ex vivo market. So when I mentioned earlier about it taking 12 months to even get past the wait list for manufacturing a virus? That applies to ex vivo, as well. So we're finding that, from a demand perspective in the industry, ex vivo delivery systems are still very valuable. Of course the eventual goal is to do in vivo, and we do have select applications that we're developing data fits for within the in vivo context, as well.
So, it's a fine balance, but from a regulatory perspective, being able to start with cell therapy approach where the FDA is already comfortable with the end product, so that you're putting the cells back in - that is a good point to show that your delivery system is safe and effective. And it’s also something that there are a number of partners where you could have up to 100 or more different genetic modifications you're performing in the cells, and the goal is just to provide the supply chain and the manufacturing for all those therapies, as far as the delivery systems go.
What we're finding is that in theory, it seems easy to just modify a gene in a cell and put in back, but in reality, there are many steps to that cell therapy process. You have to take the cells out. You have to use nucleofection or electroporation where you expose the cells to a big electromagnetic field in order to permeabilize the cell membrane. And that's where you can introduce CRISPR or whichever tool you're doing the gene editing with.
But CRISPR performs cuts, it doesn't perform insertions. You're basically using molecular scissors to create a double stranded break at some part of the genome. We then need to actually insert a new DNA sequence into that spot. The industry is typically using electroporation for the deletion part, and then they're manufacturing viruses to insert the genes back. Within that process, you also have to have very specialized conditions for growing those cells, because you actually have to grow them for typically three to six weeks.
So, you need the time between taking those cells out of the patient and putting them back in. And during that period, there are a number of steps for activating T-cells, that are also very complex and cumbersome. And the whole process ends up costing about $270,000 just for the manufacturing component for a player like Novartis.
And the drug's going to price at $470,000. So that is a really big bottleneck. Where if you can reduce the amount of steps required to engineer the cells, and make it more that you're taking the cells out, putting some nanoparticles on them, and then putting them back in; where there are only one or two steps, you're looking at major cost and time saving across the whole industry. Then you can also use those techniques for in vivo therapies, so the delivery system itself is designed to be used in vivo as well.
Andre: Well, certainly in vivo is a huge bottleneck. But we're seeing that the bottleneck is even in the ex vivo market. So when I mentioned earlier about it taking 12 months to even get past the wait list for manufacturing a virus? That applies to ex vivo, as well. So we're finding that, from a demand perspective in the industry, ex vivo delivery systems are still very valuable. Of course the eventual goal is to do in vivo, and we do have select applications that we're developing data fits for within the in vivo context, as well.
So, it's a fine balance, but from a regulatory perspective, being able to start with cell therapy approach where the FDA is already comfortable with the end product, so that you're putting the cells back in - that is a good point to show that your delivery system is safe and effective. And it’s also something that there are a number of partners where you could have up to 100 or more different genetic modifications you're performing in the cells, and the goal is just to provide the supply chain and the manufacturing for all those therapies, as far as the delivery systems go.
What we're finding is that in theory, it seems easy to just modify a gene in a cell and put in back, but in reality, there are many steps to that cell therapy process. You have to take the cells out. You have to use nucleofection or electroporation where you expose the cells to a big electromagnetic field in order to permeabilize the cell membrane. And that's where you can introduce CRISPR or whichever tool you're doing the gene editing with.
But CRISPR performs cuts, it doesn't perform insertions. You're basically using molecular scissors to create a double stranded break at some part of the genome. We then need to actually insert a new DNA sequence into that spot. The industry is typically using electroporation for the deletion part, and then they're manufacturing viruses to insert the genes back. Within that process, you also have to have very specialized conditions for growing those cells, because you actually have to grow them for typically three to six weeks.
So, you need the time between taking those cells out of the patient and putting them back in. And during that period, there are a number of steps for activating T-cells, that are also very complex and cumbersome. And the whole process ends up costing about $270,000 just for the manufacturing component for a player like Novartis.
And the drug's going to price at $470,000. So that is a really big bottleneck. Where if you can reduce the amount of steps required to engineer the cells, and make it more that you're taking the cells out, putting some nanoparticles on them, and then putting them back in; where there are only one or two steps, you're looking at major cost and time saving across the whole industry. Then you can also use those techniques for in vivo therapies, so the delivery system itself is designed to be used in vivo as well.
The Long-Term Vision for Ligandal and Gene Therapy Efficacy
Where is this company and this field going in the near future? What can we look forward to in terms of future developments with CRISPR.
Minu: What would you say is the long term vision of Ligandal? One is obviously to make gene therapy real, but is the cost factor also an important part in your strategy?
Andre: We want to take the amount of time required to confer some new genetic traits to a cell down to days. We want it to be so easy to modify a cell, either in a dish or inside the body, that you can simply say what sequence you want, and within a few days you have something that targets the right cell and delivers that sequence.
The vision of the company is to be at the forefront of personalized medicine, both through partnering and eventually through our own therapeutic development programs. But we're really staging how we go about that, in order to validate the platforms for the right kind of applications that give us long-term value for these personalized medicine approaches for really taking on aging, for doing things that aren't necessarily going to have the immediate market upside, but once you get the data sets, it's going to be very valuable.
We want to actually have sort of the ‘zip codes’ and the ‘addresses’ of the body mapped out so well, so that we can really quickly take on new application at a fraction of the cost and a fraction of the time.
Minu: That's really a great vision, and I do hope you guys achieve it. One general question would be that I know your company was founded in 2013 when CRISPR was already around, though not as big as it is now. So when you saw CRISPR becoming even more popular, did that impact your strategy or the way you work at Ligandal, or had you kind of already factored this in that gene editing tools were going to be big in the future?
Andre: Well, we knew the field would blow up, the question was when and in which applications. So when we were starting a company and trying to explain what we were doing, people didn't know what CRISPR was. They vaguely sometimes knew nanoparticles, but not in really a gene therapy context. And so coupling those things with being speculative as opposed to a foregone industry conclusion that this is where it's going to go.
It was really around 2016/2017, that the market started to shift. We started to see gene therapy approved in 2017. So suddenly, even something like viruses, which were in all sorts of clinical trials for gene therapy but weren't approved, were seen as “okay, this works.” We know that we can use an adeno-associated virus for any number of gene therapy applications, and the FDA has shown precedent in approving it, with a Spark's blindness therapy, Luxturna.
But then the oncology stuff also really took off. Where you're modifying T-cells to basically have targeting molecules for cancer, that wasn't mainstream until the last two years. Even though there were a number of companies like Kite and Juno developing these programs, or even Cellectis developing treatments for leukemia, the amount of patients that had been dosed was very small.
Now we have the first approval, we have a number of things that are getting fast tracked, and moved through to clinical trials. It's less speculative and there's now this big demand for delivery systems where people have established a precedent that you can do it. But now it's a question of can you do it faster, can you do it cheaper, can you do it for more applications.
Minu: Here on CRISPR Cuts, we like to end with a fun question: If you woke up tomorrow and you couldn't be the CEO of Ligandal, but you could be the CEO of some other biotech company, which one would that be? Like any promising ones that would be your second choice?Andre: That's an interesting question. I'd probably kick Paul out of his spot at Synthego.
Minu: Okay. Perfect. I think he would take it as a compliment, hopefully. Great.
Andre: Love you, Paul.
Andre: That's an interesting question. I'd probably kick Paul out of his spot at Synthego.
Minu: Okay. Perfect. I think he would take it as a compliment, hopefully. Great.
Andre: Love you, Paul.
Other CRISPR and Gene Therapy Podcasts You May Enjoy
If you’re looking for new podcasts all about CRISPR or genome engineering, check out our ranking of the top CRISPR podcasts, and our big list of the best science podcasts to keep yourself up-to-date with new developments. We also listed a few here that you may enjoy if you liked this episode:
Avery Posey | CAR T Therapy: Treating Cancer with Engineered Cells (with Podcast)
This topic was mentioned a number of times in this article, so if you want to learn more about T-cell therapy and how it will replace chemotherapy as the main treatment for cancer, check out our conversation with Avery Posey.
Genetically Engineered Cows: How CRISPR Could Improve Cattle Farming (with Podcast)
In this CRISPR Cuts podcast episode, learn about how a project to genetically engineer cows without horns is helping to save the beef and cattle industry, that could be in great danger without this revolutionary tool.
TED Talks Science & Medicine | How CRISPR Lets Us Edit Our DNA
In this general intro to CRISPR given by Jennifer Doudna in a TED Talk, learn the basics of how CRISPR was discovered, how it works, and what it means for the future.
Andrew Porterfield | CRISPR in the Grocery Store
In another episode of CRISPR Cuts, learn more about how soon CRISPR foods could be hitting the grocery store shelves near you, and what this means for the future of the food industry.
If you want to learn more about CRISPR, be sure to check out our big list of the best CRISPR news sources to keep on top of any new developments!
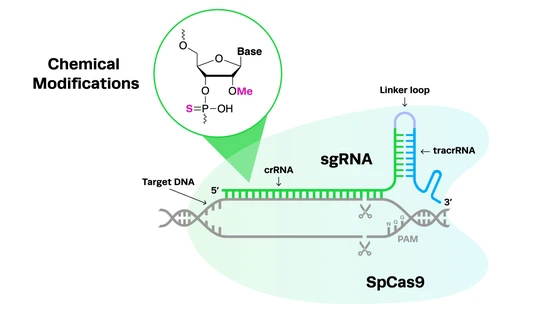
Research to GMP-grade sgRNA: From Discovery to the Clinic
Synthego is your trusted partner for CRISPR gene editing. With our comprehensive range of sgRNA quality options—large-scale RUO, INDe, and GMP—we are poised to help guide your CRISPR-based research successfully through early-phase research to your clinical application.