Contents
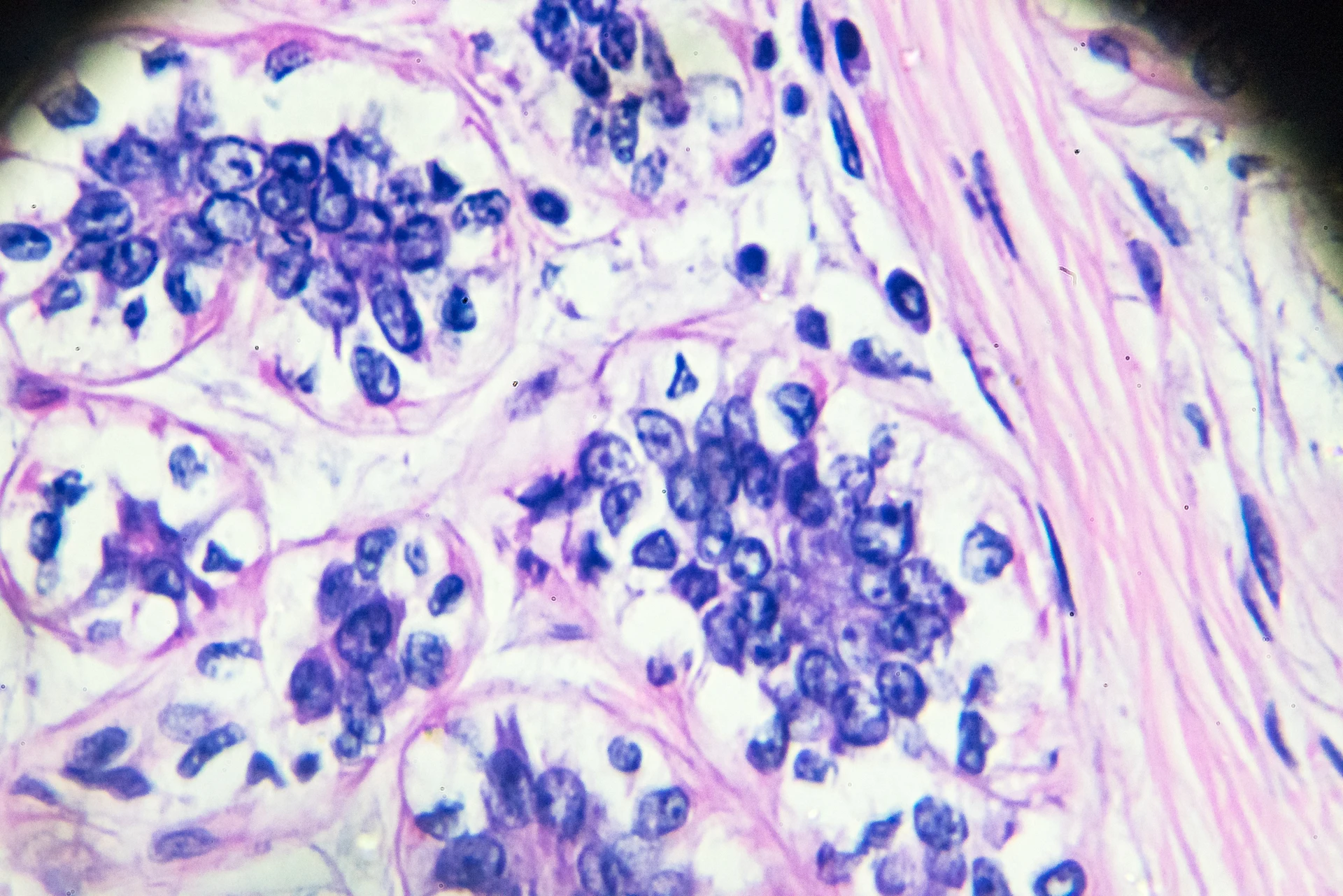
Cancer cells, both immortalized cell lines and primary cancer cells, are invaluable biological tools. They have enabled many significant breakthroughs in oncology research, and continue to be incredibly useful, particularly in the CRISPR era.
In this article, we’ll answer common questions about cancer cell lines and discuss many key aspects of cancer cell line research, including CRISPR cancer cell lines.
Cancer Cell lines: An Overview
Cancer cell lines are in vitro model systems used in place of primary cells to study biological processes. In this section, we’ll briefly discuss what cancer cell lines are, the pros and cons of immortalized cell lines, the difference between immortalized cell lines and primary cells, and mutations in cancer cell lines.
What are cancer cell lines?Cancer cell lines are cell lines that consist of “immortal” cancer cells that continually divide and grow over time under laboratory conditions. Human cancer cell lines are most commonly used to study cancer biology, identify new treatments and improve the efficacy of existing cancer treatments.
CRISPR is used frequently in many different cancer cell lines across multiple areas of research. Many researchers generate CRISPR knockouts or CRISPR knock-ins of specific genes for functional research. It can also be used to correct pathogenic point mutations in these cell lines. CRISPR interference (CRISPRi) and CRISPR activation (CRISPRa) are also commonly performed in these cells to either reduce or increase the expression of relevant genes.
Cancer cell lines are cell lines that consist of “immortal” cancer cells that continually divide and grow over time under laboratory conditions. Human cancer cell lines are most commonly used to study cancer biology, identify new treatments and improve the efficacy of existing cancer treatments.
CRISPR is used frequently in many different cancer cell lines across multiple areas of research. Many researchers generate CRISPR knockouts or CRISPR knock-ins of specific genes for functional research. It can also be used to correct pathogenic point mutations in these cell lines. CRISPR interference (CRISPRi) and CRISPR activation (CRISPRa) are also commonly performed in these cells to either reduce or increase the expression of relevant genes.
What are primary cancer cells?Primary cancer cells are cells taken directly from cancerous tissue and used for in vitro experiments. These cells cannot grow indefinitely in a laboratory setting. Since they are not cultured for extended periods, they are more biologically representative of the tumor from which they are originally derived.
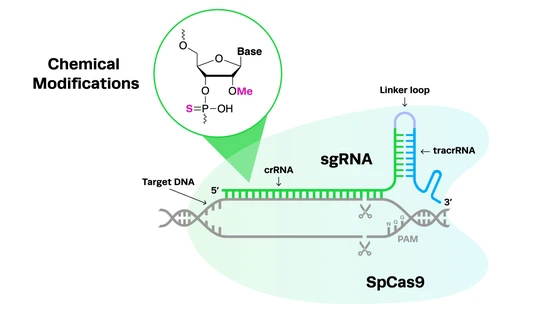
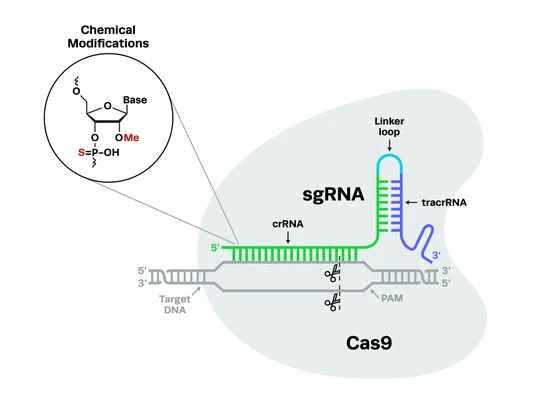
Primary cells are typically less amenable to gene editing than immortalized cell lines for a variety of reasons. However, advances in CRISPR technology are making editing primary cells much easier. A key example of this is the addition of chemical modifications to synthetic guide RNAs, to increase editing efficiencies.
Primary cancer cells are cells taken directly from cancerous tissue and used for in vitro experiments. These cells cannot grow indefinitely in a laboratory setting. Since they are not cultured for extended periods, they are more biologically representative of the tumor from which they are originally derived.
Primary cells are typically less amenable to gene editing than immortalized cell lines for a variety of reasons. However, advances in CRISPR technology are making editing primary cells much easier. A key example of this is the addition of chemical modifications to synthetic guide RNAs, to increase editing efficiencies.
Superior Quality and Editing Performance of Synthetic sgRNAs
This application note demonstrates the superior quality and editing performance of Synthego’s chemically modified sgRNAs relative to modified sgRNAs from Vendor D.

Cancer cell lines vs. primary cancer cells: what’s the difference?The key difference between immortal cancer cell lines and primary cancer cells lies in their genetic makeup. Genomic instability is a key feature of cancers, and the majority of primary tumors contain substantial heterogeneity as they are made up of multiple subclones. This heterogeneity is one of the reasons for tumor recurrence; different subclones within a tumor respond differently to various treatments, and resistant cells can therefore remain post-treatment.
In contrast, immortalized cancer cell lines are typically dominated by a single clone, hence they lack the heterogeneity of the original tumor from which they were isolated. They are also prone to genetic drift when cultured for long periods of time, meaning that they are not representative of the true responses of cancers to treatments and therapies. This has led to many studies using primary cancer cells and panels of immortal cancer cell lines to study drug efficacy, rather than focusing on an individual cell line.
As mentioned above, immortalized cell lines are much more amenable to genetic modification with CRISPR and other genome engineering technologies than primary cells. Recent advances in the CRISPR methods are making the editing of primary cells more feasible, however, and there are now a wide range of studies using CRISPR in both immortal and primary cancer cell lines.
The key difference between immortal cancer cell lines and primary cancer cells lies in their genetic makeup. Genomic instability is a key feature of cancers, and the majority of primary tumors contain substantial heterogeneity as they are made up of multiple subclones. This heterogeneity is one of the reasons for tumor recurrence; different subclones within a tumor respond differently to various treatments, and resistant cells can therefore remain post-treatment.
In contrast, immortalized cancer cell lines are typically dominated by a single clone, hence they lack the heterogeneity of the original tumor from which they were isolated. They are also prone to genetic drift when cultured for long periods of time, meaning that they are not representative of the true responses of cancers to treatments and therapies. This has led to many studies using primary cancer cells and panels of immortal cancer cell lines to study drug efficacy, rather than focusing on an individual cell line.
As mentioned above, immortalized cell lines are much more amenable to genetic modification with CRISPR and other genome engineering technologies than primary cells. Recent advances in the CRISPR methods are making the editing of primary cells more feasible, however, and there are now a wide range of studies using CRISPR in both immortal and primary cancer cell lines.
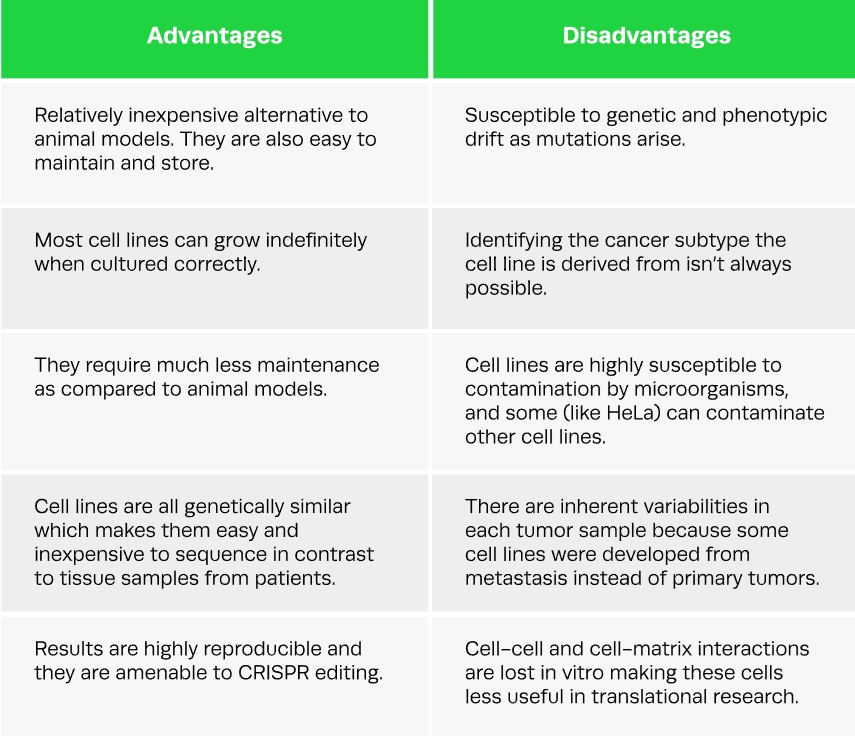
Pros and Cons of immortalized cancer cell linesSince the HeLa cell line was first discovered over 60 years ago, human cancer cell lines have become extremely popular in scientific research, particularly now that CRISPR can be used to edit their genomes. However, these cell lines do come with potential drawbacks. In this section, we’ll take a quick look at the pros and cons of cancer cell lines.Table 1. Pros and cons of using immortalized cancer cell lines in research.
Since the HeLa cell line was first discovered over 60 years ago, human cancer cell lines have become extremely popular in scientific research, particularly now that CRISPR can be used to edit their genomes. However, these cell lines do come with potential drawbacks. In this section, we’ll take a quick look at the pros and cons of cancer cell lines.Table 1. Pros and cons of using immortalized cancer cell lines in research.
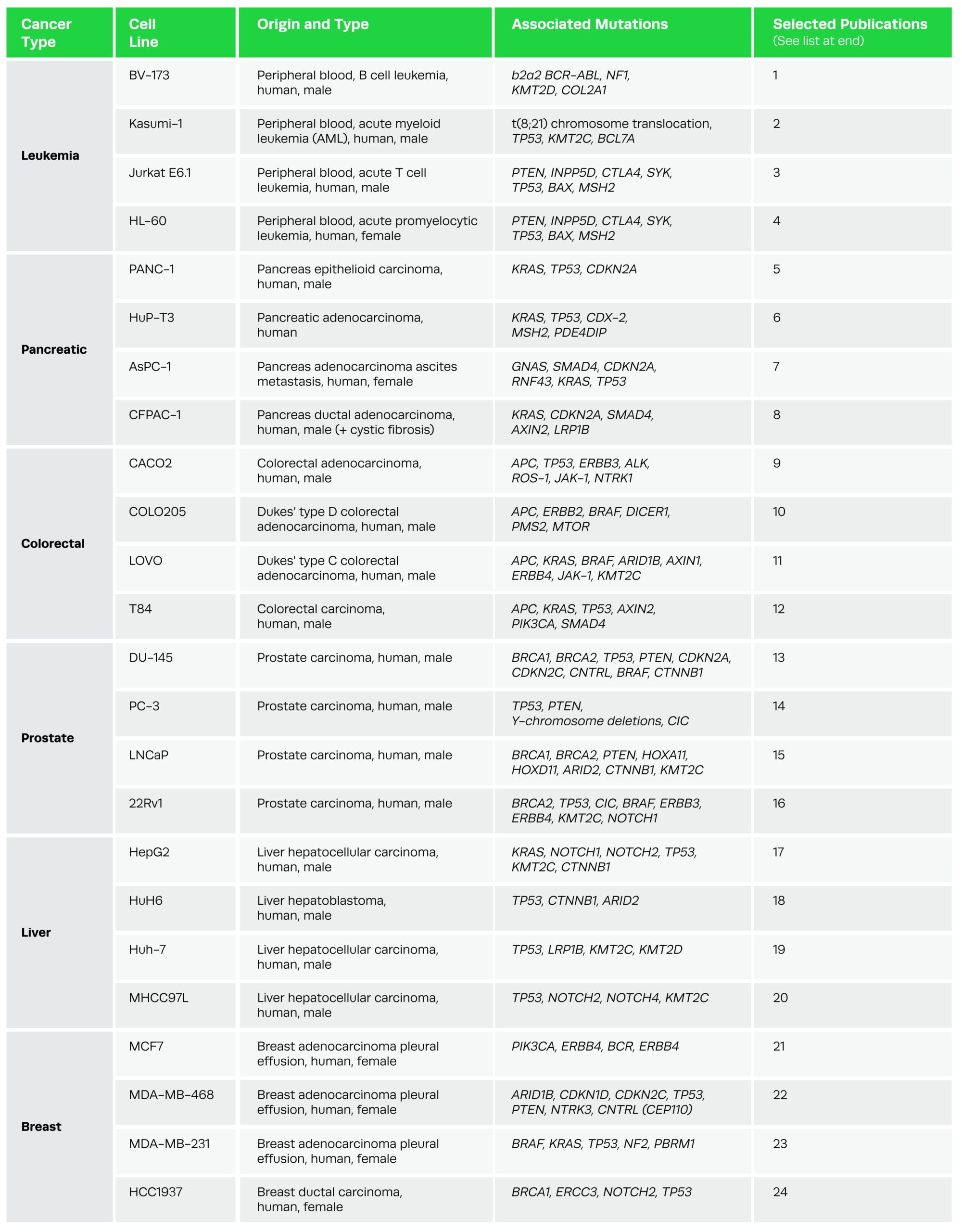
Common mutations in cancer cell lines One of the defining features of human cancer cell lines is their mutations. Mutations contributing to the pathogenesis of cancer fall into two categories: tumor suppressor genes and oncogenes. Tumor suppressors assist in the repair of damaged DNA and apoptosis, preventing normal cells from becoming cancer cells; mutations in these genes result in the uncontrolled growth of cancerous cells. In contrast, oncogenes are genes that normally control cell division when their expression is regulated (proto-oncogenes); when mutations occur in these genes, they are continually activated.
You’ll notice several of the mutations listed in the cell line tables below. Those found in the tumor suppressor gene TP53, or the oncogene KRAS, for example, are common to many of the cell lines listed, because these mutations are present in many different types of cancers. Other mutations, like those in the BRCA1 and BRCA2 genes, despite their notoriety, are significantly rarer. One of the key ways that CRISPR can be used in cancer research is to correct the pathogenic mutations in these cell lines.
One of the defining features of human cancer cell lines is their mutations. Mutations contributing to the pathogenesis of cancer fall into two categories: tumor suppressor genes and oncogenes. Tumor suppressors assist in the repair of damaged DNA and apoptosis, preventing normal cells from becoming cancer cells; mutations in these genes result in the uncontrolled growth of cancerous cells. In contrast, oncogenes are genes that normally control cell division when their expression is regulated (proto-oncogenes); when mutations occur in these genes, they are continually activated.
You’ll notice several of the mutations listed in the cell line tables below. Those found in the tumor suppressor gene TP53, or the oncogene KRAS, for example, are common to many of the cell lines listed, because these mutations are present in many different types of cancers. Other mutations, like those in the BRCA1 and BRCA2 genes, despite their notoriety, are significantly rarer. One of the key ways that CRISPR can be used in cancer research is to correct the pathogenic mutations in these cell lines.
Cell Lines for 6 Different Types of Common Cancer Types
There are hundreds of different types of cancer cell lines, encompassing a variety of disease states. Today, cell line repositories and commercial suppliers have a multitude of cancer cell lines available and can even supply panels of cell lines for various types of cancer. In this section, we’ll take a look at some of the key categories of cancer cell lines, their associated mutations, and some of the applications of these in research. Many of the cell lines listed are not from the primary tumor site but from metastases.
Resource Tips
- For more information on cancer cell lines, you can visit the Broad Institute’s Cancer Cell Line Encyclopedia.
- To investigate more mutations associated with any particular cancer or cell line, you can search the Wellcome Sanger Institute’s COSMIC Database or check out the NIH National Cancer Institute’s Cancer Genome Atlas Program.
- For details of culturing requirements for many different types of cancer cell lines, you can download Gibco and ThermoFisher’s cancer cell culture basics handbook.
- For more information on cancer cell lines, you can visit the Broad Institute’s Cancer Cell Line Encyclopedia.
- To investigate more mutations associated with any particular cancer or cell line, you can search the Wellcome Sanger Institute’s COSMIC Database or check out the NIH National Cancer Institute’s Cancer Genome Atlas Program.
- For details of culturing requirements for many different types of cancer cell lines, you can download Gibco and ThermoFisher’s cancer cell culture basics handbook.
1. Leukemia cell linesLeukemia covers many different types of cancer that affect blood cells. Most leukemia cell lines originate from peripheral blood, and an extensive range of these cell lines is available covering specific mutations and genes, such as clusters of differentiation (CD) or immunoglobulin light chain genes.
Applications: A panel of 100 leukemia cell lines, known as the LL-100 panel, has been recently developed for blood cancer studies, comprising 22 leukemia and lymphoma entities such as T-cell, B-cell, and myeloid malignancies. Panels like LL-100 are more likely to capture the full spectrum of these cancers, elucidating the function of oncogenes and potentially yielding new treatments.
Leukemia covers many different types of cancer that affect blood cells. Most leukemia cell lines originate from peripheral blood, and an extensive range of these cell lines is available covering specific mutations and genes, such as clusters of differentiation (CD) or immunoglobulin light chain genes.
Applications: A panel of 100 leukemia cell lines, known as the LL-100 panel, has been recently developed for blood cancer studies, comprising 22 leukemia and lymphoma entities such as T-cell, B-cell, and myeloid malignancies. Panels like LL-100 are more likely to capture the full spectrum of these cancers, elucidating the function of oncogenes and potentially yielding new treatments.
2. Pancreatic cancer cell linesPancreatic cancer is one of the leading causes of mortality due to cancer. Pancreatic cancer can originate either from the exocrine or the endocrine region of the pancreas. Cell lines such as PANC-1, PSN1, and AR42J were established from exocrine tumors whereas cell lines such as CRI-G5, CRI-D11, and CRI-D2 originated from endocrine tumors.
Applications: Cell lines have been used to develop in vitro models of pancreatic cancer for translational studies. These are powerful tools that can help identify potential molecular targets for therapeutic intervention as well as for the evaluation of novel drug candidates. Pancreatic cell lines have also been used for a number of toxicity studies and in the development of xenograft models for cancer.
Pancreatic cancer is one of the leading causes of mortality due to cancer. Pancreatic cancer can originate either from the exocrine or the endocrine region of the pancreas. Cell lines such as PANC-1, PSN1, and AR42J were established from exocrine tumors whereas cell lines such as CRI-G5, CRI-D11, and CRI-D2 originated from endocrine tumors.
Applications: Cell lines have been used to develop in vitro models of pancreatic cancer for translational studies. These are powerful tools that can help identify potential molecular targets for therapeutic intervention as well as for the evaluation of novel drug candidates. Pancreatic cell lines have also been used for a number of toxicity studies and in the development of xenograft models for cancer.
3. Colorectal cancer cell linesColorectal cancer (CRC) is a common type of cancer and has high mortality rates. Most CRCs are adenocarcinomas and as such, most CRC cell lines are derived from this type of cancer. There are many common mutations associated with CRC cell lines, including KRAS, TP53, and PTEN, which occur with a frequency of more than 30%.
Applications: CRC cell lines are put to use in a wide variety of oncology research areas, including growth factor signaling, target identification, drug response, targeted drug delivery, cell migration, disease pathogenesis, metastasis, and novel treatment evaluation studies. These versatile cell lines are also regularly utilized in studies of other non-cancerous colon conditions, including inflammatory bowel diseases like Crohn’s disease and leaky gut. Recently, HT-29 tumor spheroids were infected with CRC-associated anaerobic bacteria Fusobacterium nucleatum, in order to investigate the role of the bacteria in CRC progression.
Colorectal cancer (CRC) is a common type of cancer and has high mortality rates. Most CRCs are adenocarcinomas and as such, most CRC cell lines are derived from this type of cancer. There are many common mutations associated with CRC cell lines, including KRAS, TP53, and PTEN, which occur with a frequency of more than 30%.
Applications: CRC cell lines are put to use in a wide variety of oncology research areas, including growth factor signaling, target identification, drug response, targeted drug delivery, cell migration, disease pathogenesis, metastasis, and novel treatment evaluation studies. These versatile cell lines are also regularly utilized in studies of other non-cancerous colon conditions, including inflammatory bowel diseases like Crohn’s disease and leaky gut. Recently, HT-29 tumor spheroids were infected with CRC-associated anaerobic bacteria Fusobacterium nucleatum, in order to investigate the role of the bacteria in CRC progression.
4. Prostate cancer cell linesProstate cancer is the second most common cancer in men in the US and an estimated 248,530 new cases will be diagnosed during 2021. It is highly heterogeneous, in terms of both its genetics and other key biological characteristics. Only a small number of immortalized prostate cancer cell lines are available, two of which display mutations in the BRCA genes commonly associated with breast cancer. DU-145, PC-3, and LNCaP are the most commonly used prostate cancer cell lines.
Applications: Prostate cancer cell lines are used to study a variety of treatment options and screen potential drug candidates, as well as to elucidate the mechanisms of disease pathogenesis and drug resistance. Since prostate cancer is osteogenic, cell lines like LNCaP have been used for cancer progression and bone metastasis research. Androgen dependence studies are also a key application of PC cell lines as androgen deprivation therapy is a common treatment option and the androgen receptor signaling cascade is frequently altered in prostate cancers. Recently, all four of the cell lines listed below, along with others, have been used to create organoids as precision models of the complex prostate cancer microenvironment.
Prostate cancer is the second most common cancer in men in the US and an estimated 248,530 new cases will be diagnosed during 2021. It is highly heterogeneous, in terms of both its genetics and other key biological characteristics. Only a small number of immortalized prostate cancer cell lines are available, two of which display mutations in the BRCA genes commonly associated with breast cancer. DU-145, PC-3, and LNCaP are the most commonly used prostate cancer cell lines.
Applications: Prostate cancer cell lines are used to study a variety of treatment options and screen potential drug candidates, as well as to elucidate the mechanisms of disease pathogenesis and drug resistance. Since prostate cancer is osteogenic, cell lines like LNCaP have been used for cancer progression and bone metastasis research. Androgen dependence studies are also a key application of PC cell lines as androgen deprivation therapy is a common treatment option and the androgen receptor signaling cascade is frequently altered in prostate cancers. Recently, all four of the cell lines listed below, along with others, have been used to create organoids as precision models of the complex prostate cancer microenvironment.
5. Liver cancer cell linesLiver cancer is the sixth most common type of cancer and has high mortality rates. Hepatocellular carcinoma is the most common, accounting for >80% of liver cancers, the leading risk factor for which is chronic cirrhosis induced by hepatitis B or C. Less common liver cancers include cholangiocarcinoma and angiosarcoma.
Applications: Due to the fact that many cases of liver cancer arise from hepatitis-induced cirrhosis, liver cancer cell lines are commonly used for studies of hepatitis infection and life cycle. Other uses include testing potential cytotoxic effects of plant extracts and chemical compounds, determining modes of disease pathogenesis, screening drugs in metastasis studies, developing xenograft models of liver cancer, miRNA regulation research, and interferon-α sensitivity studies.
Liver cancer is the sixth most common type of cancer and has high mortality rates. Hepatocellular carcinoma is the most common, accounting for >80% of liver cancers, the leading risk factor for which is chronic cirrhosis induced by hepatitis B or C. Less common liver cancers include cholangiocarcinoma and angiosarcoma.
Applications: Due to the fact that many cases of liver cancer arise from hepatitis-induced cirrhosis, liver cancer cell lines are commonly used for studies of hepatitis infection and life cycle. Other uses include testing potential cytotoxic effects of plant extracts and chemical compounds, determining modes of disease pathogenesis, screening drugs in metastasis studies, developing xenograft models of liver cancer, miRNA regulation research, and interferon-α sensitivity studies.
6. Breast cancer cell linesBreast cancer is the most common cause of cancer-related death for women in the US. 5-10% of breast cancer cases are caused by mutations in the well-known BRCA1 and BRCA2 genes. These genes are often referred to as tumor suppressors and produce proteins that assist in the repair of damaged DNA. Mutations in BRCA genes are also associated with several other types of cancers. Since breast cancer is such a complex and heterogeneous disease, finding cell lines that are accurate experimental models can be challenging. BT20 was the first established breast cancer cell line, while MCF7 is the most widely used.
Breast cancer is the most common cause of cancer-related death for women in the US. 5-10% of breast cancer cases are caused by mutations in the well-known BRCA1 and BRCA2 genes. These genes are often referred to as tumor suppressors and produce proteins that assist in the repair of damaged DNA. Mutations in BRCA genes are also associated with several other types of cancers. Since breast cancer is such a complex and heterogeneous disease, finding cell lines that are accurate experimental models can be challenging. BT20 was the first established breast cancer cell line, while MCF7 is the most widely used.
Applications: Breast cancer cell lines are used to study endocrine therapies for breast cancer, drug resistance research, and pathophysiology, and for the generation of xenograft models. Studies of the genomic and transcriptomic profiles of breast cancer cell lines have also enabled the identification of molecular targets for specific therapies. They have also been utilized in DNA methylation studies.
The table below shows examples of different cell lines under each of these cancer types, along with common known mutations associated with these cancers.
Applications of CRISPR in Cancer Cell Lines
The advent of CRISPR genome engineering technology has enabled many breakthroughs in the field of oncology. In this section, we’ll look at some of the key examples of CRISPR cancer cell lines and how they have assisted with drug discovery, generated treatments for drug-resistant cancers, cell and gene therapies, and immuno-oncology.
Drug discovery in cancer
Previous drug discovery screens of cancer cell line panels relied on RNA interference (RNAi) via short hairpin RNA (shRNA). More recently, CRISPR has allowed researchers to perform more robust cell screens, identifying many novel targets. CRISPR-based screens have uncovered a swathe of cancer genes responsible for signaling, cell differentiation, survival, and regulatory processes, many of which have potential as drug targets. CRISPR has also led to the discovery of genetic dependencies in cancer cells and genes involved in cancer drug resistance.
Similar to the field of infectious diseases, a critical barrier to curing cancer is drug resistance. Many types of tumors cannot be cured, even when treated with complex regimens of surgery, radiotherapy, and polychemotherapy. As such, the focus of much cancer treatment research has recently shifted toward identifying and disrupting the mechanisms which allow normal cells to become cancerous, and enable resistance to treatment.
In lung cancer, for example, drug resistance has been correlated with the upregulation of certain genes, including Nuclear Factor Erythroid 2-Related Factor (NRF2). NRF2 is responsible for the regulation of several hundred other genes, which are involved in cellular stress responses. Using CRISPR, a recent study performed knockouts of NRF2 in the A549 lung cancer cell line, resulting in reduced proliferation of cells and increased sensitivity to chemotherapy treatment. The study confirmed the results of the cell line experiments in a xenograft mouse model, where NRF2 knockout cells displayed significantly reduced rates of proliferation - even in the absence of chemotherapy treatment.
Precision disease modelingWhile cancer cell lines are useful in their own right, CRISPR has served to make them even more advantageous. Since cancer genomes are incredibly complex and vary between patients, precision models are a necessity in order to understand tumor biology and develop more effective treatments.
Complex models bearing all the necessary mutations, deletions, and chromosomal abnormalities can now be generated fairly rapidly and efficiently using CRISPR. Examples include engineering human intestinal organoids to create models of colorectal cancer and acute models of myeloid leukemia generated from mouse hematopoietic stem cells (HSCs).
CRISPR can confirm causative roles for genetic mutations in genes of interest, such as oncogenes and tumor suppressor genes. It is also frequently used to identify genes that are essential for the growth and survival of cancer cell lines, like PANC-1, which is a model for pancreatic cancers. In the breast cancer cell line MCF7, CRISPR has been used to knock in functional copies of the FOXA1 transcription factor gene.
Creating drug-resistant cellular models is also critical in cancer research, but is typically a painstakingly slow and laborious process with low efficiencies. This is an area in which CRISPR has enabled significant and rapid advances, reducing timescales from years to weeks. In a 2018 study, researchers used CRISPR to generate knockouts of the mediator complex subunit 12 (MED12) gene in multiple cancer cell lines, creating resistant models for drug screening. These models can be used to determine the efficacy of anti-cancer drugs and combinations of these for treating drug-resistant tumors.
CRISPR has also been used to generate specific mutations in the epidermal growth factor receptor (EGFR) gene in the PC9 lung cancer cell lineg. The mutation in question, T790M, is known to cause resistance to tyrosine kinase inhibitors, which are usually effective treatment options for lung adenocarcinomas. Creating CRISPR-edited cancer cell lines like this allows researchers to investigate both drug efficacy and the mechanisms of drug resistance in mutated cells.
Some cancers, such as acute myeloid leukemia and Ewing’s sarcoma, are caused by chromosomal translocations. Despite the clear need to study these in a disease model to generate more effective treatments, they have been difficult to recapitulate. CRISPR has now enabled these cancer-related chromosomal aberrations to be generated in nearly any cell line, however, allowing research on these types of cancers to progress rapidly.
While cancer cell lines are useful in their own right, CRISPR has served to make them even more advantageous. Since cancer genomes are incredibly complex and vary between patients, precision models are a necessity in order to understand tumor biology and develop more effective treatments.
Complex models bearing all the necessary mutations, deletions, and chromosomal abnormalities can now be generated fairly rapidly and efficiently using CRISPR. Examples include engineering human intestinal organoids to create models of colorectal cancer and acute models of myeloid leukemia generated from mouse hematopoietic stem cells (HSCs).
CRISPR can confirm causative roles for genetic mutations in genes of interest, such as oncogenes and tumor suppressor genes. It is also frequently used to identify genes that are essential for the growth and survival of cancer cell lines, like PANC-1, which is a model for pancreatic cancers. In the breast cancer cell line MCF7, CRISPR has been used to knock in functional copies of the FOXA1 transcription factor gene.
Creating drug-resistant cellular models is also critical in cancer research, but is typically a painstakingly slow and laborious process with low efficiencies. This is an area in which CRISPR has enabled significant and rapid advances, reducing timescales from years to weeks. In a 2018 study, researchers used CRISPR to generate knockouts of the mediator complex subunit 12 (MED12) gene in multiple cancer cell lines, creating resistant models for drug screening. These models can be used to determine the efficacy of anti-cancer drugs and combinations of these for treating drug-resistant tumors.
CRISPR has also been used to generate specific mutations in the epidermal growth factor receptor (EGFR) gene in the PC9 lung cancer cell lineg. The mutation in question, T790M, is known to cause resistance to tyrosine kinase inhibitors, which are usually effective treatment options for lung adenocarcinomas. Creating CRISPR-edited cancer cell lines like this allows researchers to investigate both drug efficacy and the mechanisms of drug resistance in mutated cells.
Some cancers, such as acute myeloid leukemia and Ewing’s sarcoma, are caused by chromosomal translocations. Despite the clear need to study these in a disease model to generate more effective treatments, they have been difficult to recapitulate. CRISPR has now enabled these cancer-related chromosomal aberrations to be generated in nearly any cell line, however, allowing research on these types of cancers to progress rapidly.
CRISPR studies for understanding gene function in cancer There have been many recent studies examining the effects of gene knockouts on cancer cells in an effort to identify potential targets for cell and gene therapy. In ovarian cancer research, the gene ONECUT Homeobox 2 (OC-2), a transcription factor, was found to be highly expressed in ovarian cancer tissues and cell lines and was implicated in tumor progression. A recent study used CRISPR-Cas9 to knockout OC-2used CRISPR-Cas9 to knockout OC-2 in SKOV3 and CAO3 cells, leading to downregulation of several pro-angiogenic growth factors, suppression of tumor growth, and apoptosis.
Mutations in the proto-oncogene Kras have been detected in 90% of pancreatic ductal adenocarcinoma cases, making it another key target for CRISPR-based cancer treatment. A 2019 study used CRISPR-Cas9 to knock out heterozygous Kras mutations in three different cell lines, followed by an analysis of changes in signal transduction proteins, with the knockout cells resembling wild-type cells in terms of expression of signal transduction genes. This study both confirms Kras can be targeted to restore normal cell function and that specific knockdowns of Kras can be performed using CRISPR.
Progress has also been made toward finding a cure for cervical cancer using CRISPR-Cas9. Human papillomavirus (HPV) causes many cases of cervical cancer via degradation of p53, a tumor suppressor gene, by the HPV E6 oncoprotein. In a key study, CRISPR-Cas9 was used to perform knockouts of E6 in three HPV-positive cervical cancer cell lines. Subsequent analysis of genetic mutations, mutation frequency, protein expression levels, apoptosis, and cell proliferation revealed downregulation of E6, upregulation of p53, increased levels of apoptosis, and dose-dependent suppression of cell growth. An in vivo mouse model was then used to explore the effects of treatment in subcutaneous tumors - intratumoral administration resulted in significant suppression of tumor growth with no adverse events detected.
Other studies have used CRISPR with different Cas nucleases to provide potential gene therapies for cancer. A notable example is a 2020 paper which used CRISPR-Cas13a to knock out endogenous oncogenes such as TERT in the liver cancer cell line HepG2. As a result, the cell line displayed significant apoptosis and reduced growth, indicating that CRISPR editing of TERT and other oncogenes can be used as a treatment for liver cancer.
There have been many recent studies examining the effects of gene knockouts on cancer cells in an effort to identify potential targets for cell and gene therapy. In ovarian cancer research, the gene ONECUT Homeobox 2 (OC-2), a transcription factor, was found to be highly expressed in ovarian cancer tissues and cell lines and was implicated in tumor progression. A recent study used CRISPR-Cas9 to knockout OC-2used CRISPR-Cas9 to knockout OC-2 in SKOV3 and CAO3 cells, leading to downregulation of several pro-angiogenic growth factors, suppression of tumor growth, and apoptosis.
Mutations in the proto-oncogene Kras have been detected in 90% of pancreatic ductal adenocarcinoma cases, making it another key target for CRISPR-based cancer treatment. A 2019 study used CRISPR-Cas9 to knock out heterozygous Kras mutations in three different cell lines, followed by an analysis of changes in signal transduction proteins, with the knockout cells resembling wild-type cells in terms of expression of signal transduction genes. This study both confirms Kras can be targeted to restore normal cell function and that specific knockdowns of Kras can be performed using CRISPR.
Progress has also been made toward finding a cure for cervical cancer using CRISPR-Cas9. Human papillomavirus (HPV) causes many cases of cervical cancer via degradation of p53, a tumor suppressor gene, by the HPV E6 oncoprotein. In a key study, CRISPR-Cas9 was used to perform knockouts of E6 in three HPV-positive cervical cancer cell lines. Subsequent analysis of genetic mutations, mutation frequency, protein expression levels, apoptosis, and cell proliferation revealed downregulation of E6, upregulation of p53, increased levels of apoptosis, and dose-dependent suppression of cell growth. An in vivo mouse model was then used to explore the effects of treatment in subcutaneous tumors - intratumoral administration resulted in significant suppression of tumor growth with no adverse events detected.
Other studies have used CRISPR with different Cas nucleases to provide potential gene therapies for cancer. A notable example is a 2020 paper which used CRISPR-Cas13a to knock out endogenous oncogenes such as TERT in the liver cancer cell line HepG2. As a result, the cell line displayed significant apoptosis and reduced growth, indicating that CRISPR editing of TERT and other oncogenes can be used as a treatment for liver cancer.
Immuno-oncology researchOne of the most significant recent advances in cancer treatment research has been in CAR T cell therapy. This involves collecting the T cells of a cancer patient, activating and engineering them, using a retroviral vector, to express chimeric antigen receptors that are specific to antigens from their own tumor cells. When expanded and re-infused back into the patient as CAR T cells, they will identify, attack, and eliminate cancerous cells. This is a highly patient-specific treatment, however, and to overcome this limitation, CRISPR is now being used to develop universal CAR T cells that can be used for any patient.
One of the most significant recent advances in cancer treatment research has been in CAR T cell therapy. This involves collecting the T cells of a cancer patient, activating and engineering them, using a retroviral vector, to express chimeric antigen receptors that are specific to antigens from their own tumor cells. When expanded and re-infused back into the patient as CAR T cells, they will identify, attack, and eliminate cancerous cells. This is a highly patient-specific treatment, however, and to overcome this limitation, CRISPR is now being used to develop universal CAR T cells that can be used for any patient.
For more information on how CAR T therapy is being developed and the role of CRISPR, you can check out our CRISPR Cuts podcast interview with Avery Posey, an expert in T cell engineering and cancer immunotherapy. There are currently several clinical trials underway using CRISPR-engineered CAR T cells to treat patients suffering from B cell cancers and multiple myeloma.
CAR T Therapy: Treating Cancer with Engineered Cells (with Podcast)
Synthego sits down with Avery Posey, leading the charge on CAR T cell therapy research and bringing this technology to cancer patients as soon as possible. Learn how CAR T works, what stage it’s in now, and how it will help revolutionize the treatment of cancer.
CRISPR Editing is Advancing Cancer Cell Line Research
CRISPR gene editing in human subjects is still in its infancy, and researchers have proceeded cautiously when it comes to clinical trials for gene therapies that could potentially cure cancer. However, CRISPR has many other applications that will contribute to cancer research.
There are many hurdles throughout the process of clinical development for potential cancer treatments and cures, often due to the fact that immortalized cell lines used in pre-clinical research do not always accurately reflect the biological complexity of disease in human subjects. Since CRISPR is able to produce complex edits in so many different types of cells, immortalized CRISPR cancer cell lines will become increasingly relevant models of disease in the coming years, likely accelerating the process of clinical trials and minimizing trial failures.
Advances are constantly being made in the realm of CRISPR technology, including the discovery and engineering of new Cas nucleases, tailoring of methods to reduce off-target effects of gene editing, and the optimization of CRISPR delivery mehods. These improvements will make it safer and more feasible to apply CRISPR directly to human subjects in order to cure cancer and other diseases.
The next few years will no doubt see an increase in the number of clinical trials using CRISPR to treat various cancers, including by engineering immune cells to make them better able to detect and kill cancerous cells. In addition, high-throughput CRISPR screens have enabled the identification of many genes which may contribute to oncogenesis, which will, in turn, lead to novel treatments for these cancers.
We hope this guide helped you understand more about cancer cell lines, the variety of cancer cell lines available, and how they can be used in research, particularly when engineered with CRISPR-Cas9. If you have questions about engineered cancer cell lines or are interested in using them in your research, you can contact one of our genome-engineering experts for more information.
Selected Cell Line-Specific Publications
Leukemia
- BV-173: Schubert et al. 2010, Dillman et al. 2009, Christova et al. 2013.
- Kasumi-1: Dan et al. 2014, Mpakou et al. 2013, Hernandez et al. 2017.
- Jurkat E6.1: Gioia et al. 2018, Abraham & Weiss, 2004, Basaiyye et al. 2018.
- HL-60: Christova et al. 2013, Asik et al. 2018, Yu, Liu & Gu, 2021.
- BV-173: Schubert et al. 2010, Dillman et al. 2009, Christova et al. 2013.
- Kasumi-1: Dan et al. 2014, Mpakou et al. 2013, Hernandez et al. 2017.
- Jurkat E6.1: Gioia et al. 2018, Abraham & Weiss, 2004, Basaiyye et al. 2018.
- HL-60: Christova et al. 2013, Asik et al. 2018, Yu, Liu & Gu, 2021.
Pancreatic cancer
- PANC-1: Malinda et al. 2020, Ma et al. 2019, Zhao et al. 2018.
- HuP-T3: Anastasiadou et al. 2020, Li et al. 2017, Ohshima et al. 2018.
- AsPC-1: Zhao et al. 2018, Bakke et al. 2019, Khodavirdipour et al. 2020.
- CFPAC-1: Petrella et al. 2017, Kim et al. 2020, Zhou et al. 2019.
- PANC-1: Malinda et al. 2020, Ma et al. 2019, Zhao et al. 2018.
- HuP-T3: Anastasiadou et al. 2020, Li et al. 2017, Ohshima et al. 2018.
- AsPC-1: Zhao et al. 2018, Bakke et al. 2019, Khodavirdipour et al. 2020.
- CFPAC-1: Petrella et al. 2017, Kim et al. 2020, Zhou et al. 2019.
Colorectal Cancer
Prostate Cancer
Liver Cancer
- HepG2: Xu et al. 2020, Zhao et al. 2020, Badroon et al. 2020.
- HuH6: Whitlock et al. 2020, Zheng et al. 2020, Eloranta et al. 2020.
- Huh-7: Wu et al. 2020, Yu et al. 2020, Afify et al. 2020.
- MHCC97L: Ma et al. 2020, Ding et al. 2020, Wang et al. 2021.
- HepG2: Xu et al. 2020, Zhao et al. 2020, Badroon et al. 2020.
- HuH6: Whitlock et al. 2020, Zheng et al. 2020, Eloranta et al. 2020.
- Huh-7: Wu et al. 2020, Yu et al. 2020, Afify et al. 2020.
- MHCC97L: Ma et al. 2020, Ding et al. 2020, Wang et al. 2021.
Breast Cancer
- MCF7: Zhang et al. 2020, Hazman et al. 2021, Hasan et al 2020.
- MDA-MB-468: Bauer et al. 2020, Niu et al. 2020, Barragán-Cárdenas et al. 2020.
- MDA-MB-231: Si et al. 2020, Arisan et al. 2021, Benot-Dominguez et al. 2021.
- HCC1937: Young et al. 2020, Xu et al. 2020, Alvarado-Cruz et al. 2021.
- MCF7: Zhang et al. 2020, Hazman et al. 2021, Hasan et al 2020.
- MDA-MB-468: Bauer et al. 2020, Niu et al. 2020, Barragán-Cárdenas et al. 2020.
- MDA-MB-231: Si et al. 2020, Arisan et al. 2021, Benot-Dominguez et al. 2021.
- HCC1937: Young et al. 2020, Xu et al. 2020, Alvarado-Cruz et al. 2021.